A woman in her 50s with past medical history of heart failure, prior stroke, atrial fibrillation on Eliquis, lung cancer in remission, and CKD, presented to the emergency department for evaluation of cough and shortness of breath. EKG was obtained in triage and read as ventricular bigeminy. What do you think?
On my first read of the EKG, I agreed with the initial interpretation. Pendell Meyers then recommended that I take a second look at the morphology of the QRS complexes. I think it was easiest for me to see in the rhythm strip, but there are clearly P waves in front of every QRS complex.
So what is the QRS morphology below?
Enlarging a singular beat highlights a clear P wave with a shortened PR interval and slurred upstroke to the R wave. I think it is easy to see now that the QRS is widened because of an accessory conduction pathway. In context of our original EKG, the patient appears to be alternating conduction through the AV node and accessory pathway - a condition previously described as Wolf-Parkinson-White Alternans.[1]
If we look at the patient’s previous EKG on record, we’re able to see that this pattern is not new:
Interestingly, the patient does appear to have PVCs in this ECG as well as WPW beats. If we zoom in, we can see a QRS complex with slurred upstroke and shortened PR interval, a PVC which has no slurring to the upstroke of the R wave, followed by another beat down the accessory pathway.
If we enlarge lead II, we can see a distinct difference between the accessory pathway conduction and the PVC.
Here there is a P wave with a slurred upstroke to the R wave and shortened PR-interval. Notice that there is no P wave in front of the subsequent beat and steeper upstroke of the R wave. The two beats have clearly distinct morphologies and appropriately different T waves.
Ultimately, our patient was determined to have a mild CHF exacerbation and diuresed well in response to IV furosemide. She never had an oxygen requirement or tachydysrhythmia. She was informed of her accessory pathway, which had previously been undiagnosed. The patient already had an ICD in place and was discharged home with recommendations to follow up with her cardiologist.
Learning Points:
Accessory pathways can conduct intermittently. Additionally, some accessory pathways can conduct anterograde (from atria to ventricles), retrograde (from V to A), or both. There is a wide variety of locations, function, and effect on the QRS complex seen in WPW.
WPW can cause abnormal depolarization that causes abnormal repolarization, which can both mimic and conceal ischemic findings.
Other WPW-related cases:
A 19 year old with panic attacks. On the previous ECG, the diagnosis was missed, as it frequently is!
WPW mimicking and obscuring acute MI (5 Cases)
12 Year Old Asthmatic with Intermittent Dyspnea Unresponsive to Albuterol---What is it, and Why Now?
"Concealed WPW"
Interestingly, the delta wave may not always be seen! If the accessory pathway is far enough from the SA node, the depolarization from the SA node may not reach the accessory pathway by the time the AV node depolarizes. This results in no delta wave! However, you can "uncover" the accessory pathway by slowing the rate down in these patients. Another way that WPW can be concealed is in the very rare (~15% of all WPW patients) retrograde-only conduction, in which the accessory pathway ONLY allows retrograde conduction, which obviously wouldn't show a delta wave on sinus EKG but still predisposes the patient to re-entry tachycardias.
For more on concealed conduction:
Other cases involving AF with WPW:
A 47-year-old man with abdominal pain and heart rates approaching 300 bpm
Here is a relevant and tough case of intermittent runs of antidromic AVRT:
Wide Complex Tachycardia: is the patient stable or unstable?
References:
1. Khouzam RN. Wolf-Parkinson-White alternans diagnosis unveiled by adenosine stress test. J Electrocardiol. 2010 Mar-Apr;43(2):144-5. doi: 10.1016/j.jelectrocard.2009.09.002. Epub 2009 Sep 29. PMID: 19793587.
===================================
MY Comment, by KEN GRAUER, MD (11/19/2022):
===================================
Recognition of WPW can be challenging. This is especially true in selected cases of intermittent preexcitation — in which AP (Accessory Pathway) conduction may closely resemble ventricular ectopy. To enhance the above intriguing discussion by Drs. Nicholson and Meyers — I focus my comment on a few additional points to facilitate this distinction.
- For clarity of illustration — I've selected the latter segment of the long lead II rhythm strip from the 2nd 12-lead ECG shown in today's case (Figure-1).
QUESTION:
- How does the timing of beats #6 and 8 (that are conducted with preexcitation) — differ from the timing of the PVC ( = beat #9)?
-USE.png) |
| Figure-1: How does the timing of beats #6 and 8 (that are conducted with preexcitation) — differ from the timing of the PVC ( = beat #9)? |
ANSWER:
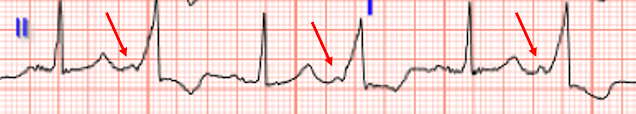
To emphasize — Assessment of this tracing is made difficult because there is an underlying sinus arrhythmia and, because P wave amplitude is small.
- RED arrows are placed at the beginning of sinus P waves on this tracing.
- As per Drs. Nicholson and Meyers — beats #6 and #8 are recognized as beats conducted with preexcitation because: i) They are preceded by seemingly on-time sinus P waves; ii) The PR interval preceding these beats is short; and, iii) The QRS complex of beats #6 and 8 is wide with initial slurring by the "signature" delta wave.
- In contrast — Beat #9 occurs earlier-than-expected — and beat #9 is not preceded by an on-time sinus P wave (ie, the WHITE arrow highlights approximately where we'd expect the next on-time sinus P wave to occur — with the slight notching under this arrow perhaps representing the end of that next sinus P wave).
Potential CAVEATS in Diagnosis:
Drs. Nicholson and Meyers emphasize that the difference between PVCs and preexcited beats in today's tracing — is that PVCs are not preceded by P waves, and PVCs lack a delta wave. But there can be caveats that may hinder this distinction.
- Preexcited beats in today's tracing are extremely wide and preceded by a very short PR interval. Thus, there appears to be complete preexcitation (ie, all impulses are traveling anterograde over the AP). But any relative percentage of conduction over the AP may occur. For example, if conduction is primarily orthodromic over the normal AV nodal pathway — then the QRS may not be overly widened, and the PR interval may not be as obviously shortened. It becomes more difficult to recognize WPW conduction when the relative amount of preexcitation is less.
- Some patients with WPW may manifest a Concertina Effect — in which there may be beat-to-beat change in the relative amount of preexcitation (CLICK HERE for an example of this phenomenon). This constant changing in the PR interval and in QRS morphology may complicate distinction between WPW conduction vs PVCs.
- Even when there is significant preexcitation — delta waves are not always obvious, and they are not always present in all leads.
- Initial slurring of the QRS complex may be seen with ventricular beats. After all — PVCs originate from anywhere within the ventricles. When the site of origin of a PVC is far from conduction tissue and/or in approximation with "scar" — delay in the form of initial slurring of the QRS may be seen.
- Not all PVCs occur "early" in the cycle. Instead — some PVCs are "end-diastolic", and may occur so late in the cardiac cycle that they are actually preceded by on-time sinus P waves.
CONFESSION: As explained by Drs. Nicholson and Meyers — there is no doubt about the distinction between WPW conduction vs the PVCs in today's case! But on occasion (despite my awareness of all of the above potential caveats) — I still find myself challenged by problematic widened beats that render me uncertain as to whether there is preexcitation or ventricular ectopy.





No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.