Case submitted by Rachel Plate MD, written by Pendell Meyers
A man in his 70s presented with chest pain which had started acutely at rest and has lasted for 2 hours. The pain was still ongoing at arrival. He also noted a bilateral "odd feeling" in his arms. He stated it was similar to prior heart attacks. He had history of prior MIs and CABG, as well as diabetes, hypertension, and hyperlipidemia.
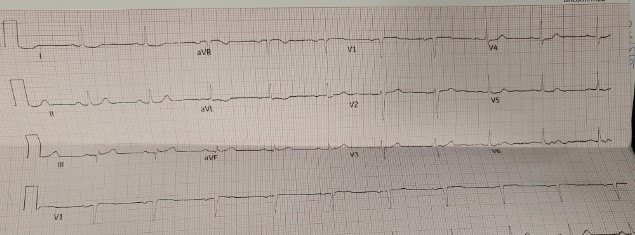
Here is his triage ECG:
PM Cardio version:
With no other information at all, I sent this ECG to Dr. Smith, who replied: "I think it is real. V3. STD in V4-5 too."
What he means is: he thinks the signs of inferior and posterior OMI are real. While the inferior findings have morphology that do not make it 100% specific (but still very concerning, especially later when the baseline is available for comparison), the combination with unexplained STD in V3-V4 (posterior OMI) makes the inferior OMI more certain as well.
In other words, this ECG shows sinus rhythm, normal QRS complex, and:
--Inferior OMI: STE in III, hyperacute T waves in lead III, reciprocal STD and TWI in aVL.
--Posterior OMI: unexplained STD max in V3-V4.
 | |
|
His initial troponin T was 15 ng/L (only two hours since pain onset).
About an hour later, he was then found on the floor in cardiac arrest in the ED. He underwent CPR and then was shocked out of VF.
 | |
|
Post ROSC 2 (about 20 minutes after ROSC):
His second troponin was 46 ng/L. No further troponins were measured.
He was taken to the cath lab where he was found to have acute total occlusion of his saphenous vein graft to his RCA, which was stented.
He was in cardiogenic shock requiring an impella for several days after cath.
12 hours post cath:
 |
He was discharged neuro intact.
Learning Points:
Although it was subtle, the initial ECG in this case can be recognized as OMI. Sooner identification likely leads to better outcomes, and in this case may have allowed prevention of cardiac arrest and better long-term outcome.
ST depression maximal in V1-V4, in the context of ACS symptoms and unexplained by QRS abnormality or tachydysrhythmia, should be considered posterior OMI until proven otherwise.
Both hyperacute T waves and posterior OMI are now formally endorsed as "STEMI equivalents" by the ACC.
===================================
MY Comment, by KEN GRAUER, MD (11/23/2022):
===================================
Cases in which initial ECG findings are subtle before undergoing dramatic change, — are always impressive. Such is the situation in today's post by Drs. Plate and Meyers. I focus my comment on these initial subtle findings.
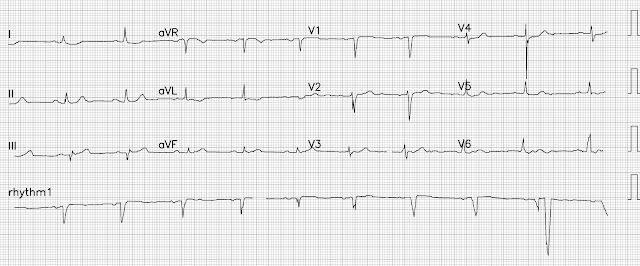
- For clarity in Figure-1 — I've reproduced the first 2 tracings in today's case.
The history in today's case — was that of a man in his 70s who presented to the ED for 2 hours of chest pain, that was still present on arrival in the ED. His initial tracing ( = ECG #1) was obtained at this time.
- Of Note: This patient had a history of prior MIs and CABG.
QUESTIONS:
About 1 hour after ECG #1 was done — the patient was found on the floor in the ED in cardiac arrest.
- In view of the above history and this patient's initial ECG shown in Figure-1 — Should you have suspected that the dramatic ST-T changes seen in the post-ROSC tracing would develop?
- When should a 2nd ECG have been done?
-USE.png) |
| Figure-1: Comparison of the initial ECG in today's case — with this patient's baseline tracing. (To improve visualization — I've digitized the original ECG using PMcardio). |
MY Thoughts on the Initial Tracing:
Clearly we could not predict that this patient would undergo cardiac arrest within an hour after arriving in the ED, with the dramatic ECG changes seen in the above post-resuscitation tracing. But we should not be surprised.
- We've shown many cases on Dr. Smith's ECG Blog of subtle ECG findings that rapidly evolve into dramatic ST-T wave changes. At times — the initial subtle findings simply represent a phase of "pseudo-normalization" that may occur soon after spontaneous reopening of an acutely occluded coronary artery. We have no idea if marked ST elevation might have preceded the ECG appearance of ECG #1 during the 2 hours before today's patient arrived in the ED.
- KEY Point: When there is uncertainty about whether an initial ECG represents "new" or "old" findings — repeating the ECG sooner rather than later (ie, within ~10-20 minutes) is one of the best ways to tell! This apparently was not done in today's case.
- Today's patient is high-risk (ie, in a high "prevalence" group for having an acute coronary event). He has known coronary disease (with previous MIs & CABG) — and he presented to the ED for new-onset chest discomfort. Even before looking at his ECG — our "mindset" needs to be to assume an acute cardiac event until we can prove otherwise.
Like Dr. Smith — I was shown this patient's initial ECG without the benefit of any clinical information. My thoughts were as follows:
- The rhythm in ECG #1 is sinus. The large Q wave in lead III (and the small q in the first complex in lead aVF) could be old from this patient's prior MIs. But the T waves in each of the inferior leads (especially in lead III) looked potentially hyperacute (ie, taller and "fatter"-at-their-peak than expected, given QRS amplitude in these leads).
- While the ST-T wave flattening in lead I, with slight T wave inversion in lead aVL do not look acute — the ST-T wave appearance in these leads is not normal, and could represent reciprocal changes.
- The overall ST-T wave appearance in the chest leads looks nonspecific — except for leads V3 and V4. The ST segments in leads V3 and V4 are clearly straightened, with a hint of slight ST depression that should not normally be seen in these leads (RED lines in Figure-1).
- BOTTOM Line: As a single ECG (ie, without benefit of any prior tracing for comparison — and even without knowledge of the history) — I thought this initial tracing raised concern about a possible acute cardiac event.
- KEY Point: While I was not initially certain that the inferior lead T waves represented hyperacute change — I knew that the ST straightening with slight depression in leads V3,V4 was not "normal". Additional information would be needed for optimal decision-making.
- Once the above history is known (ie, a high-risk patient with new-onset chest pain) — the findings in ECG #1 have to be interpreted as acute until proven otherwise!
- Once the above history is known — the need for repeating the ECG sooner rather than later (ie, within the next ~10-20 minutes) should be clear.
Comparison with the prior ECG:
- Lead-to-lead comparison of ECG #1 with a previous tracing on this patient ( = ECG #2 in Figure-1) — leaves no doubt that the subtle changes in ECG #1 are new. While the Q wave in lead III was indeed present before — T wave size and shape in each of the inferior leads was unremarkable in the prior tracing.
- ST-T waves in high-lateral leads I and aVL were simply flat on the prior tracing — compared to the slight ST depression in lead I and shallow T wave inversion in lead aVL that is present in ECG #1.
- The chest leads in the prior tracing showed nonspecific ST-T wave flattening. However, the ST segment straightening with slight depression seen in leads V3 and V4 of ECG #1 was not present in this patient's baseline ECG.
- LESSONS to be Learned: To emphasize — We clearly could not have predicted from ECG #1 that this patient was about to undergo cardiac arrest. However, given the history in this patient with known coronary disease — the ECG findings in today's initial tracing have to be assumed indicative of ongoing OMI until proven otherwise. Obtaining a repeat ECG within the next 10-20 minutes might have revealed diagnostic dynamic ST-T wave changes. And once the prior ECG became available for comparison — all doubt about the acuity of this process should have been erased.




No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.