Written by Jesse McLaren (@ECGCases), with comments by Smith and Grauer
A 50 year old presented with chest pain radiating to the shoulder. They had a history of an LAD stent 10 years ago and alcohol use disorder, with repeated visits for chest pain and two code STEMIs two years ago that found no occlusive disease.
What do you think?
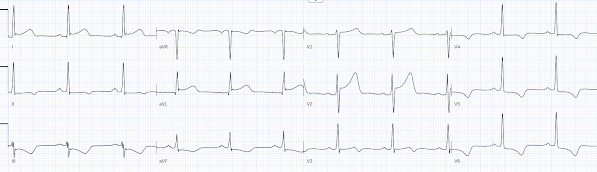
There’s normal sinus rhythm, normal intervals, normal axis, and normal R wave progression. There’s LVH with repolarization abnormalities, including discordant ST depression and T wave inversion inferolaterally and discordant ST elevation and tall T wave in V2.
Are there any primary ischemic changes? How can we identify OMI in the presence of LVH?
1. prior ECGs
Below are the first and last ECGs from that the visit resulting in a code STEMI, which found a patent LAD stent but no occlusive disease (as per the discharge summary, further angiogram details not available):
This shows the benefits and limitations of prior ECG. On the one hand, we can see prior secondary repolarization abnormalities. But we can also see that they fluctuate over time, and can vary with differences in lead placement.
2. proportionality
The secondary ST/T changes from LVH can make it difficult to assess primary ischemic abnormalities, and the STEMI paradigm doesn’t even try—defining STEMI as ST elevation in the absence of LVH. But the OMI paradigm can draw from the principle of proportionality. As Drs. Aslanger, Meyers and Smith explain in Recognizing electrocardiographically subtle occlusion myocardial infarction and differentiating it from mimics: ten steps to or away from the cath lab: “If there is high voltage indicating left ventricular hypertrophy (LVH), some STE may be seen in leads with deep S waves (usually V1-V3) and may mimic STEMI. If the amplitude of STE is more than one-sixth of the amplitude of S-wave in one of these leads, it is highly suspicious for OMI.”
This patient has a baseline ST/T ratio in V2 of >15% but it is greater on the new ECG. Both the second ECG from the last visit and new ECG have 3mm of ST elevation in V3, but the S wave has diminished from 14mm to 11mm, raising the ST/T ratio from 21% to 27%.
Very important post for understanding anterior ST Elevation in the presence of LVH:
LVH with anterior ST Elevation. When is it anterior STEMI?
3. patient
With the patient's repeated visits with chest pain, prior stable angiograms and repolarization changes on ECG, it would have been easy to dismiss. But the cardiologist was concerned about the patient’s
description of the pain, which was worse than prior episodes and in a patient with prior coronary artery disease, so they activated the cath lab. The LAD stent was patent
but there was a 90% ulcerated plaque in the right posterolateral branch, which
was stented. There was also 30% proximal RCA and 50% proximal circumflex lesions.
Because of a cath lab activation and culprit lesion requiring a stent, the patient was diagnosed as “STEMI”. But they never had a rise in troponin, and the initial and post-cath trop were the same: 14ng/L prior (normal <26 in males and <16 in females) and 13 after. So was this unstable angina?
Smith: I don't think you can even make this conclusion. It might or might not be unstable angina, probably not, and with fluctuating ECG.
Here is the post-cath ECG:
There’s the same ST elevation in V2 and similar S wave, but now the T wave seems even larger. Is this a posterior reperfusion T wave, given the location of the culprit? But there should be at least a tiny increase in troponin with reperfusion injury.
A few days later the patient presented again with chest pain, and EMS brought in again as code STEMI based on anterior ST elevation and inferior ST depression. This time the patient declined cath and serial trops remained at 13. Echo findings: "a normal size of the LV with concentric remodeling and overall normal left systolic ejection fraction. Mild anterior septum segment, mid septum segment, and mid inferior segment wall motion abnormalities were noted. RV was normal in size and function, and there was no relevant valve pathology." The patient was diagnosed with non-cardiac chest pain. Below are the initial and discharge ECGs:
Again we see some of the variations in repolarization abnormalities, exaggerated by lead placement (R/S ratio is different V2-4 and the V1-2 are placed too high on the second—with fully negative P in V1 and biphasic P in V2).
Take home
1. Problem: LVH produces secondary repolarization abnormalities which can make it difficult to identify primary ischemic changes, and STEMI criteria don’t help
2. Prior ECGs can show baseline repolarization changes, but these can fluctuate over time and with variations in lead placement and patient position
3. Proportionality: disproportionate ST elevation can help identify OMI—with ST/S>15% concerning—but there can still be false positives
4. Patient: patients with high-pretest probability and ischemic symptoms deserve investigation even if prior angiograms have been unremarkable or ECGs are nonspecific
5. Paradigm: code STEMIs leading to stents does not mean the patient had a “STEMI”. ACS should not be classified by whether the presenting ECG has ST elevation, but by whether the patient had Occlusion MI (OMI) or non-Occlusive MI (NOMI)-- or unstable angina.
Smith: How would we conclude in retrospect that this was, or was not, OMI?
1. Any ECG which manifests ischemia should have evolution. This fluctuating LVH probably would not fulfill that criterion.
2. There should be at least some troponin rise and/or fall, even if they do not reach the 99th percentile. Furthermore, it would be very rare for this to be OMI without at least one troponin going over the 99th percentile. Our research definition of OMI requires either a) diminished flow in the artery (TIMI 0-2) or b) culprit plus a very high troponin. There can be OMI that does not meet these criteria (but that does manifest on the ECG and has evolution) due to a) occlusion that is too brief, or b) inability to identify a culprit, but there must be SOME troponin rise and/or fall, even if it is unstable angina with all of them below the 99th percentile. The definition of acute MI includes a rise and/or fall of troponin with at least one value over the 99th percentile for that assay.
Therefore, this patient had Non-ischemic ST Elevation and a chronic, stable stenosis that was intervened upon. There was some non-ischemic fluctuation in the ECG.
This patient should carry around a copy of their ECG!
- The history of "alcohol use disorder". While this most definitely does not rule out the possibility of new acute cardiac disease — in my experience, it always made it more difficult for me to assess such patients.
- A series of prior ECGs on the patient that showed fluctuation of ST-T wave abnormalities. That said — differences in lead placement made assessment of these fluctuations more difficult.
- Some unusual findings on the initial ECG (including LVH) — that left me uncertain about how to proceed.
- ECG #1 shows a normal sinus rhythm at a rate just over 60/minute. The PR interval is normal, and the QRS is narrow — but the QTc is prolonged (I estimate ~480 msec.). The frontal plane axis is normal at +20 degrees.
- I have previously reviewed "My Take" on a user-friendly approach to the ECG diagnosis of LVH (See My Comments in the June 20, 2020 and April 27, 2019 posts in Dr. Smith's ECG Blog). Voltage criteria are not quite met in the chest leads in Figure-1. There are met in lead aVL (R ≥12 mm in aVL) — and the very tall R wave in lead I is probably also qualifying.
- As I've emphasized in previous posts — the fact that more there are more than 50 criteria in the literature for the ECG diagnosis of LVH means that none of these criteria are optimal. It also means that the ECG is far from a perfect assessment tool for LVH. For practical purposes — when QRS amplitude appears increased and ST-T wave changes consistent with LV "strain" are present — the probability is high that "true" LVH is present if the patient is an adult of a certain age who has a history of heart disease. I therefore thought the diagnosis of LVH to be secure.
- There was subtle ST elevation in the high-lateral leads I and aVL of ECG #1 — with what appeared to be some mirror-image opposite ST depression in the inferior leads. Could this be acute? (especially since the ST-T wave depression of LV "strain" was nowhere to be seen in these high-lateral leads?).
- There was moderately deep and symmetric T wave inversion in lateral chest leads V5,V6 (with terminal negativity of the T wave in lead V4). Was this consistent with ischemia? with LV "strain"? — or — with a combination of the two?
- My Impression of ECG #1: I was not at all certain from assessment of this initial ECG as to how I would answer Dr. McLaren question about whether to activate the cath lab. My "hunch" — was that acute OMI was less likely — but I felt I'd need more information (ie, the degree of concern from the patient's history and symptoms, comparison with other tracings, troponins, etc.) to make my decision.
- Review of the 2 prior tracings from the patient's last code STEMI visit did not resolve my uncertainty. While ST-T wave changes seemed a bit more marked on ECG #1 than on the prior tracings — I did not think they provided a definitive answer.
-USE%20copy.png) |
| Figure-1: The initial ECG in today's case. |
- Unfortunately — assessment of this patient in the future may remain problematic if he again returns for chest pain, but without definitive ECG changes or troponin elevation.
- P.S.: Very important point highlighted by Dr. Smith's last comment = Just because there is a high-grade stenosis (ie, a 90% narrowing in today's case) — does not necessarily mean that this is a "culprit" lesion responsible for symptoms.







No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.