A 40-something woman with Chest Pain of 20 minutes duration called 911.
It started while at rest and she describes it as crushing pain radiating
to the left arm. She has a history of HTN for which she takes
Lisinopril. Denies any other medical history.
She
appears well but in obvious pain. She was diaphoretic but pink
and warm. BP remained 150-160 systolic throughout care.
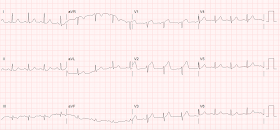
This prehospital ECG was
obtained.
 |
| There are very suspicious ST elevation and T-waves in V2, but without 2 consecutive leads with STE of greater than or equal to 1.5 mm, it does not meet STEMI criteria. |
The medic used the formula for differentiating LAD occlusion from Precordial Normal Variant ST Elevation (also commonly referred to as "Early Repolarization")
With a computerized QTc of 430, the formula value was 24.94. Since this is greater than 23.4, the ECG represents LAD occlusion with a high degree of certainty.
Because of this, they bypassed the nearest hospital and transported the patient to the nearest STEMI receiving facility, which has PCI capabilities.
On the way, they recorded 3 more ECGs:
Time 5 minutes
 |
| No major change This one was transmitted to the receiving facility, with request to activate the cath lab. The receiving physician would not activate, did not agree. |
When the emergency physician would not activate, the medic took things into his own hands and contacted the cardiologist himself. As soon as the cardiologist saw the ECG, he activated the cath lab.
2 more ECGs were recorded en route:
Time 30 minutes
 |
| Still no major change |
Time 33 minutes
 |
| Still no major change |
The patient bypassed the ED and went directly to angiogram:
 |
| After stenting, there is good flow in the LAD |
Learning Point
Subtle LAD coronary occlusion can be diagnosed by medics, especially with use of the formula. It may greatly aid in triaging patients to the appropriate hospital and aid in improving door to balloon time.


Hats off to the medics!
ReplyDeleteamazing as usual
ReplyDeleteIf you had the option, you would always take a suspicious STEMI to a facility with a Cath lab. No need for a formula there. I'm surprised the ED guys in this case blatantly refused to activate. Despite this, it would take less than 2-3 mins to SMS the ECG to a cardiologist to get a definitive opinion. I'm sure the Cardiologist did not use a formula. Where I work, we err on the side of caution when unsure and activate more often. Better for the patient.
ReplyDeleteA few points stand out to me on this ecg:
ReplyDelete1/ While some ST elevation can be expected in V1-2,it seems rather tall compared to the relatively low qrs voltage.
2/T waves look very big and "fat" - hyperacute T?
3/ There appears to be a hint of ST-depression in the inferior leads. This should be absent in BER, I would think.
So even without the formula, this does not look like a reassuring ecg.
Of course, this is a patient with chest pain, diaphoresis and that "somethings wrong" feeling. Being relatively inexperienced, I might miss this in a confused elderly patient. Not to mention that the cardiologist might be difficult to convince!
Maarten — You are RIGHT ON! You summarized in many fewer words than me what I thought were some major messages for this insightful case!
DeleteTotally agree.
DeleteThe medic should get a medal. What I most like about this is seeing someone well-trained and knowledgeable who is prepared to buck the authority gradient and do whatever needs to be done to achieve the right outcome.
ReplyDeleteI would have called that inferior ST depression sagnificant reciprocal STD in this context and bypassed the formula. Would you agree with that?
ReplyDeleteLooking forward to meet you at DASSMACC!
Well, to me the whole ECG screams LAD occlusion without the formula, but obviously not to everyone (e.g., the emergency physician). So the formula is meant for those who do not "see" is so easily. Furthermore, while there is a downsloping ST segment, the J-point is not depressed (you can be fooled by the wandering baseline).
DeleteYes, see you at SMACC!
In other news paramedic fired in retaliation. Loses house and wife. Cardiologist remains silent and goes golfing.
ReplyDeleteOuch
DeleteIf someone was fired over a decision that was made in the best interest of the patient no matter what the cath showed, the service would be doing that person a favor by firing them.
DeleteHighly insightful case that in my opinion should be “required reading” for anyone involved in acute assessment/management of patients with new chest pain. Use of Dr. Smith’s Formula clearly adds support of one’s suspicions for anyone questioning the subtle-but-very-real abnormalities seen on these serial tracings. But the goal of my comment is to emphasize ADDITIONAL reasons why the medic did well in this case to contact the Cardiologist directly.
ReplyDeleteImportant Learning Points from this Case include the following: i) Patients with new-onset worrisome chest pain who seek EMS care are a HIGH prevalence population. This means that compared to an ambulatory population of patients who describe atypical, less acute symptoms — a much greater percentage of people who contact EMS for new-onset chest pain will end up having an acute cardiac event. This means that “subtle ECG abnormalities” are MUCH more likely to be real than seeing similar ECG findings in a lower prevalence population of patients who do not have typical new-onset symptoms.
ii) Official ECG “STEMI criteria” are not perfect. They WILL have FALSE NEGATIVES in certain patients, especially early on and/or in cases in which acute coronary occlusion may be transient or intermittent. Awareness that the patient in front of you is from a “high prevalence” population should CLUE YOU IN to the need to be more accepting of subtle ECG findings.
iii) ECGs with subtle findings often have subtle findings in MORE than a single lead. Recognition of subtle findings in multiple leads supports your suspicion that the ECG is truly NOT normal. In the 1st ECG in this case — the J point is elevated no less than 3 mm in lead V2. This is more than “early repolarization” typically manifests, especially given the SMALL depth of the S wave in this lead. In addition, the T wave in lead V2 looks “fatter”-than-it-should-be. Just like the abnormality in a frank Brugada ECG pattern is an abnormality that is sometimes difficult to describe in words, but which needs to be COPIED into one’s brain — the picture seen here in lead V2 of this 1st ECG showing disproportionate ST-T wave peaking should be memorized in the brains of all who assess acute cardiac patients. But in addition, the ST-T wave in neighboring lead V1 is not normal! The T wave in lead V1 may normally be negative, positive or flat. But it should not be coved with slight elevation as seen here. So there ARE 2 consecutive leads here that clearly show subtle-but-real ST-T wave abnormalities in a “high prevalence” patient with worrisome new-onset chest pain. In addition, inferior leads III and aVF are not normal. Granted, there is not frank mirror-image ST depression in these leads — but in context of new chest pain + abnormal ST-T waves in V1,V2 — I interpret the nonspecific ST-T wave flattening that I see here in leads III and aVF as potential reciprocal changes.
iv) The way to COMPARE one ECG with a subsequent one is to put BOTH tracings right next to each other — and then to go LEAD-by-LEAD as you compare the two. Doing so for ECG #1 and ECG #2 suggests to me that there IS some progression (subtle-as it is) — in that lead V1 now shows unequivocal slight ST elevation on the 2nd ECG — and in addition to lead V2, the T wave in lead V3 is now also taller-than-it-should-be considering small size of the QRS in this lead. Seeing that there IS some progression to me confirms that these ECG findings ARE real and acute.
v) If ever we find ourselves in a situation in which we are clearly not comfortable with a decision made by a provider who is “advising us” — we should purse the case until such time that we CAN become comfortable. This tenet is not to be taken lightly, as there may be more than one correct way to manage any given patient. But, if we feel there is potential harm from the advice we are being given, then tactfully seeking another opinion is what needs to be done. Fortunately the medic in this case did so, and the Cardiologist promptly recognized the need for acute cath in this case.
THANKS to Dr. Smith for presenting this case!
ST depression and T wave inversion inferiorly show reciprocal changes making the V1 and V2 more believable. The angiogram shows some collateral circulation which is probably why the ECG was not as striking. When in doubt we always went to cath.
ReplyDeleteThanks for the case
ReplyDeleteInferior changes may be or not related to this acute LAD occlusion, but in AVF there is a subtile progression of the height of the T waves : they become quite symetric and equal to the low QRS voltage.
ReplyDeleteHave you a post stenting ECG to compare these T waves and why not the thin but deep q waves in DIII
Gilles,
DeleteIn my mind, there is no question that the inferior ST-T is due to the LAD occlusion, though subtle and I did not mention it.
Unfortunately there is no post PCI ECG.
Steve