See below for Ken Grauer Comment on the initial ECG:
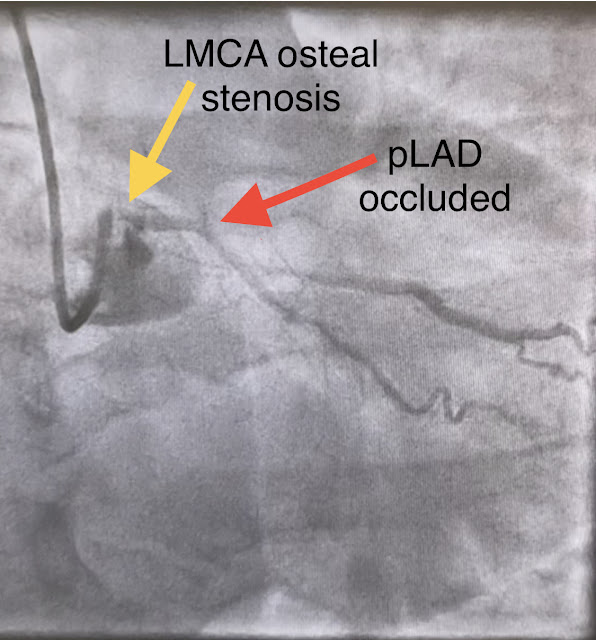
- LMCA — 90-99% osteal stenosis.
- LAD — 100% proximal occlusion; with 70-89% mid-vessel narrowing.
- LCx — 50-69% stenosis of the 1st marginal branch; with 100% distal LCx occlusion.
- RCA — 100% proximal occlussion.
The patient in today’s case presented in cardiogenic shock from proximal LAD occlusion, in conjunction with a subtotally stenosed LMCA. The RCA was occluded proximally — and was being filled retrograde from the left-sided vessels. Upon contrast injection of the LMCA, the patient deteriorated, as the LMCA was severely diseased and flow to all coronary arteries (LAD, LCx and RCA) was compromised.
Following PCI — the patient became uncooperative and agitated, and needed intubation. Over the next couple of days the patient was weaned off of mechanical circulatory support. Inotropic medication was continued. Troponin T peaked at 38,398 ng/L ( = a very large myocardial infarction)
The echo images below were obtained on the day of presentation after PCI. Cardiac function is poor, with akinesis of the LAD territory. The impella catheter is seen in the left ventricular outflow tract (LVOT).
The patient was extubated on Day-3 of the hospital stay. Unfortunately, he required re-intubation a few days later due to respiratory distress from severe bilateral pneumonia. The stay in the cardiac intensive care unit (CICU) was further complicated by sepsis, delirium, GI bleeding, and anuric renal failure with need for renal replacement therapy.
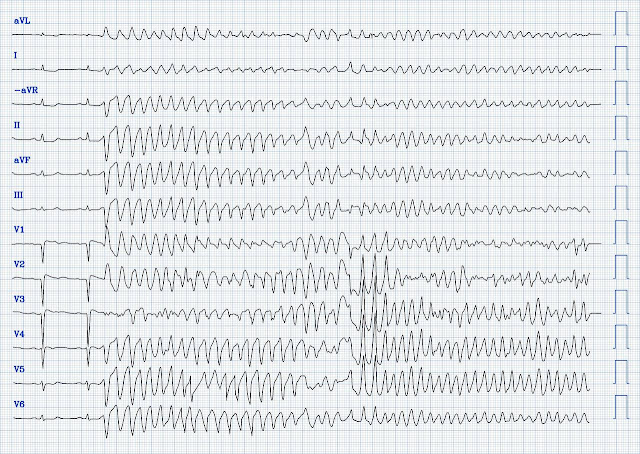
The patient improved, and on Day-11 of the hospital stay — he was off inotropes and on a small dose of a ß-blocker. However, he suddenly developed a series of malignant ventricular arrhythmias. This progressed to electrical storm, with incessant PolyMorphic Ventricular Tachycardia (PMVT) and recurrent episodes of Ventricular Fibrillation (VFib). He required multiple defibrillations within a period of a few hours. Below are printouts of some of the arrhythmias recorded. What do you think?
===============================
Discussion:
Today's patient manifests multiple episodes of PMVT and VFib. Sinus-conducted beats in the above examples show a normal QTc interval. This is an important finding related to the etiology and treatment of these malignant arrhythmias — since by definition, PMVT with a prolonged QTc is classified as Torsades de Pointes (and entails different treatment recommendations).
The schematic grouping below reviews classification of PMVT types:
In today's case — the sinus-conducted beats prior to and between the episode of PMVT show evidence of completed anterior wall MI. That said — there is no evidence on ECG of re-occlusion of the infarct artery. In both tracings — an exceedingly fast PMVT is documented. The arrhythmia starts with a PVC having a short coupling interval. The R-R intervals of the VT are less than 200ms and ventricular rate > 300 bpm! (Distinction of PMVT vs VFib is an academic one in this case). Both PMVT and VFib occurred multiple times. Some episodes of PMVT would terminate spontaneously — but on many occasions, the PMVT degenerated to VFib, requiring defibrillation.
The situation in today's case was of a critically ill young man with an exceedingly electrically unstable myocardium. Simply stated — the patient was having recurrent PMVT without QTc prolongation, and without evidence of ongoing transmural ischemia. (If there had been ECG findings indicating reocclusion of the artery — an angiogram would have been warranted). Some residual ischemia in the infarct border might still be present. There was no evidence bradycardia leading up to the runs of PMVT (as tends to occur with Torsades). If there had been — a temporary atrial pacemaker could have been considered as a way of increasing the heart rate to suppress a bradycardia-dependent arrhythmia ("overdrive pacing").
QUESTION:
- How will you handle this arrhythmia given the clinical scenario?
NOTE: This patient was already on a low-dose ß-blocker. IV Amiodarone was ordered — but did not reduce the frequency of ventricular ectopics or the number of VT episodes. The patient continued in arrhythmic storm with recurring PMVT and VFib episodes.
- What are additional treatment options?
Our Thoughts:
- In contrast, conventional treatment of this type of ventricular arrhythmia with agents including ß-blockers, Amiodarone, Magnesium and Lidocaine — all-too-often fails.
- Studies of patients with coronary artery disease who developed arrhythmic storm with episodes of PMVT following MI — show arrhythmias indistinguishable from those reported in this case. In such cases — radiofrequency ablation of ectopic beats triggering malignant ventricular arrhythmias was needed for control of arrhythmic storm because the antiarrhythmic medications tried were ineffective (Marrouche et al — JACC 5;43(9): 1715-20, 2004).
- Of interest — the ectopic beats triggering PMVT/VFib in such studies were often mapped to endocardial sites displaying Purkinje potentials within the myocardial scar — suggesting potential responsivity to a 1A agent (Nogami — Pacing Clin Electrophysiol 34(8): 1034-1049, 2011).
Today's patient was started on oral Quinidine-Sulfate (400mg x 4/day) — with a rapid cessation of all PMVT and VFib episodes. In a case like today’s all contraindications are relative if the drug you are giving is effective as the underlying entity you are treating is deadly if not controlled.
The most common side effects of Quinidine is hypotension and QTc prolongation. These are also the most commonly reported findings in toxic overdoses with ventricular arrhythmias being reported as the leading cause of death. Information is scarce when it comes to what constitutes a toxic dose. Numbers given are based mostly on case reposts. Lethality reported from ingestion of 5 grams in a toddler while survival after ingestion of 8 grams has been reported in an adolescent.
What About Procainamide?
The PROCAMIO study included hemodynamically stable patients in VT. In this study — Procainamide was superior to Amiodarone for terminating monomorphic VT, as well as having fewer adverse effects than Amiodarone (Ortiz et al — Eur Heart J 1;38 (17): 1329-1335, 2017).
Procainamide, like Quinidine is a Type 1A antiarrhythmic. Because Procainamide is not marketed in Norway — I have no experience using this agent.
- In the United States (and in other locations where Quinidine is not readily available) — Procainamide would seem the recommended choice to consider for arrhythmias like those in today's case, especially if not responding to the usual antiarrhythmic regimen.
===============================
Smith comment: I agree with starting with a beta blocker such as esmolol, since this is likely to be a hyper-catecholaminergic state. Another approach is sympathetic chain (stellate ganglion) blockade if you have the skills to do it: it requires some expertise and ultrasound guidance. If these do not work, the a type 1a anti-dysrhythmic is certainly a reasonable choice (procainamide, or in Norway, quinidine). Administration of Procainamide is 10-17 mg/kg at 20 mg/min. A 1000 mg dose will take 50 minutes.) One should infuse until: 1) good effect, or 2) hypotension or 3) increase in QRS duration to 1.5x baseline (this is what most recommend but seems like far too much QRS widening to me)
===============================
See these articles and this graphic:
2. Stellate ganglion blockade for the management of ventricular arrhythmia storm
CASE Conclusion:
Today's patient ultimately made a full recovery — and was discharged home. An ICD (Implantable Cardioverter Defibrilator) was placed prior to discharge. Quinidine eventually was discontinued due to development of hemolytic anemia. Additional follow-up was not available.
Learning points
- PMVT following MI can be very difficult to treat. Quinidine (or perhaps Procainamide if Quinidine not available) might be considered as an option for refractory cases, especially if other methods tried were not effective.
- When dealing with recurrent episodes of PMVT — attention to the QTc interval of sinus-conducted beats is essential for distinction between Torsades vs other types of PMVT.
See this article on polymorphic VT
This review of anti arrhythmic drugs is worth a read
MY Comment, by KEN GRAUER, MD (7/21/2024):
- I focus my comment on the initial ECG in today's case — which I've reproduced and labeled in Figure-1.
- The pattern of at the very least proximal LAD occlusion — is evident from marked ST elevation beginning in lead V1 — attaining peak amplitude in lead V2 — and continuing until lead V4.
- Proximal left coronary artery occlusion is supported from limb lead findings of marked ST elevation in lead aVL (with a hyperacute ST-T wave in lead I) — and even more dramtic reciprocal ST depression in each of the inferior leads.
- Cath findings shown above in Dr. Nossen's discussion confirm multi-vessel disease, including 90-99% osteal stenosis of the LMCA. As we've often emphasized on Dr. Smith's ECG Blog — it is rare in practice to see LMCA occlusion, because most such patients die before reaching the hospital. Nevertheless, this entity does occur on occasion — and it is important to appreciate its ECG presentation. As I review in My Comment in the January 16, 2020 post of Dr. Smith's ECG Blog (and have reproduced in Figure-2 below) — the ECG of patients with acute LMCA occlusion may be varied. Today's extensive ST-T wave elevation and depression (with ST elevation in lead aVR) — is consistent with one of these patterns.
- Precordial "Swirl" — for which Drs. Meyers and Smith illustrate 20 example cases vs "look-alikes" of Swirl (with my synthesis of "Swirl" ECG findings in My Comment on that post) from October 15, 2022. In Figure-1 from today's case — the coved ST elevation in lead V1 vs the nearly mirror-image opposite ST depression in lead V6 present as marked an example of acute septal ischemia as I've encountered.
- T-QRS-D (Terminal-QRS-Distortion) — with my RED arrows highlighting as marked an example of T-QRS-D as I've encountered. Drs. Smith and Meyers emphasize that this ECG finding is diagnostic of acute OMI when seen in leads V2 and/or V3 (and probably also in lead V4) — though the picture of T-QRS-D seen in lead aVL of Figure-1 clearly tells a similar story (See My Comment at the bottom of the page in the November 14, 2019 post in Dr. Smith's ECG Blog — for illustrative description of T-QRS-D).
-USE-labeled.png) |
| Figure-1: I've labeled the initial ECG in today's case. (To improve visualization — I've digitized the original ECG using PMcardio). |
 |
| Figure-2: Reasons for the varied ECG presentation of acute LMain occlusion — excerpted from Dr. Smith’s 8/9/2019 post (See text). |
Addendum Note:
Quinidine has a long history of use to treat cardiac arrhythmias and severe malaria. My understanding is that the IV formulation of Quinidine is no longer readily available (if manufactured at all) in the US. In today's patient (who was treated in Norway) — Oral Quinidine was used.
- Oral Quinidine is available in sulfate or gluconate formulations. Rapid-acting oral formulations begin to work within 1-3 hours. The most common adverse effects are GI (diarrhea, nausea, vomiting) — and these are usually drug limiting.
- Principal adverse cardiac effects of Quinidine include QRS widening and QTc prolongation. With longterm use there may be — bradycardia, AV conduction defects and risk of Torsades de Pointes (especially in patients also on Digoxin). Other adverse effects may be seen (Today's patient ultimately stopped the drug due to hemolytic anemia).
- Although used extensively as an antiarrhythmic agent in the past in the U.S. — the adverse effect profile of Quindine, and the greater efficacy of other antiarrhythmic agents have limited longterm Quinidine use (at least in the U.S.) for this purpose. That said — the drug worked wonders for treatment of today's patient! (who had otherwise resistant ventricular arrhythmias!).
IV Procainamide is used in the United States.
- During the years that I used the drug — the dosing regimen I favored was to give 100 mg IV slowly over 5 minutes (at ~20 mg/minute) — until one of the following end points is reached: i) The arrhythmia is suppressed; ii) Hypotension occurs; iii) The QRS widens by 50%; — and/or — iv) A total loading dose of 500-1,000 mg has been given. This may be followed with IV infusion at 2 mg/minute (1-4 mg/minute range).
- NOTE: Although the maximal rate for IV Procainamide infusion has been limited to 50 mg/minute — adverse effects (ie, hypotension, bradycardia, QRS widening) are less at slower infusion rates (ie, of ~20 mg/minute).







No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.