A patient was found down approximately 30 minutes after taking methamphetamine. Bystander CPR. Medics found patient in PEA arrest. He was resuscitated into a perfusing rhythm. He went in and out of arrest until arrival at the ED.
Here is the only prehospital 12-lead:
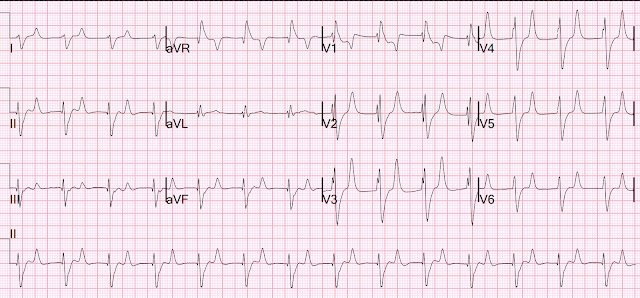
Here is the first ED ECG:
This ECG is pathognomonic of hyperkalemia, with wide QRS, very SHARPLY peaked T-waves, flat ST segments, RBBB pattern and large R-wave in aVR.
What does that say about the rhythm? It is regular. It is supraventricular. It is not tachycardic.
Is this an accelerated Junctional rhythm? Junctional rhythm is possible, but most likely is "Sinoventricular rhythm". Sinoventricular rhythm is a supraventricular rhythm that is initiated by the sinus node but does not manifest with P-waves because the hyperkalemia completely flattens the P-wave.
The K returned at 7.8 mEq/L.
Core temp was 40 degrees C.
The remaineder of the case was complicated and the patient ultimately died.
See here another case of sinoventricular rhythm:
And more cases discussing Sinoventricular Rhythm:
https://hqmeded-ecg.blogspot.com/search/label/Sinoventricular%20Rhythm
MY Comment, by KEN GRAUER, MD (4/30/2024):
- For clarity in Figure-1 — I've labeled the 2 ECGs in today's case.
- I fully acknowledge some speculation — given that we lack precise timing of these serial tracings, as well as not knowing the corresponding serum K+ level at the time each tracing was recorded.
- To EMPHASIZE: The points that I discuss below that relate to the rhythm in ECG #1 and ECG #2 — are advanced concepts that go beyond-the-Core!
-USE.png) |
| Figure-1: I've labeled the 2 ECGs in today's case. |
- Whereas this truncation of QRS amplitudes does not affect clinical management in today's case — we have shown a number of examples in which anterior lead ST elevation might suggest acute LAD OMI if one was not aware that such ST-T waves would not be disproportionate IF full anterior lead S wave amplitude was recorded (See My Comment at the bottom of the page in the November 29, 2023 post and in the June 20, 2020 post in Dr. Smith's ECG Blog).
- PEARL #1: With an SVT rhythm — Consider the possibility of 2:1 conduction IF you see equally spaced, similar P-wave-looking deflections. Use of calipers immediately provides the answer — that these upright, peaked deflections seen in each of the inferior leads are not equally spaced (measuring 360 msec. vs 320 msec.) — and therefore, the dark BLUE line deflection in lead II is not an "extra" P wave.
- Similarly — the upright peaked light BLUE line deflection immersed within the depressed ST segment in lead II also can not be an "extra" P wave — because there clearly is no way this peaked light BLUE line deflection could produce a regular tachycardic P wave rate with other pointed deflections in this rhythm.
- PEARL #2: At times like this, when I am initially uncertain whether the upright peaked deflections are part of the ST-T wave vs "extra" P waves — LOOK for the "break" in the rhythm (which occurs after the 3rd beat). Doing so should make it clear that the peaked light and dark BLUE deflections in Figure-1 are related to the preceding QRS complex (and not to the next QRS complex).
- BOTTOM Line: As bizarre as it initially might seem — these extra upright peaked deflections seen in each of the inferior leads of ECG #1 do not represent atrial activity. Instead — these peaked deflections represent part of the ST-T wave! This is relevant to interpretation of the initial (EMS) ECG in today's case — as I explain momentarily!
- Applying PEARLS #1,2,3 to today's case — and, knowing that the extra peaked deflections in ECG #1 are part of the ST-T wave (and do not represent "extra" atrial activity) — should suggest hyperkalemia from this initial ECG!
- I say this because: i) Today's clinical setting of metamphetamine toxicity leading to PEA arrest may predispose to hyperkalemia via mechanisms of rhabdomyolysis and acute renal failure (Gurel — Clinical Case Reports 4(3):226, 2016); and, ii) Parts of upright T waves that are seen in ECG #1 are tall, upright, peaked and pointed (RED arrows in ECG #1 — especially in lead V3) — whereas many leads show the mirror-image opposite picture of deep, negative T waves that are pointed with a narrow base (BLUE arrows in ECG #1). As per PEARL #3 — pointed T waves that are inverted instead of upright are an important ECG sign of hyperkalemia.
- That said — Note (as per PEARL #3) that 2 of the leads in ECG #2 show the mirror-image opposite picture of slender, pointed T waves that are inverted (BLUE arrows in ECG #2).
- Are we certain there is a sinoventricular rhythm in ECG #2?
- Doesn't the QRS complex in ECG #2 look very different — compared to morphology of the fairly narrow QRS in ECG #1?
- Why are almost all of the the pointed T waves with narrow base upright in ECG #2? — whereas T waves in ECG #1 were biphasic with a predominantly negative T wave?
- PEARL #4: I do not think we can reliably distinguish between sinoventricular vs accelerated idioventricular rhythm in ECG #2. That said — PEARL #4 is that clinically (as I emphasize in the February 27, 2023 post) — Most of the time it does not matter what the rhythm disturbance is with hyperkalemia — because: i) Arrhythmias tend not to "obey the rules" when there is marked hyperkalemia; and, ii) Rhythm disturbances from hyperkalemia usually improve (or completely resolve) as soon as IV calcium is administered.



No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.