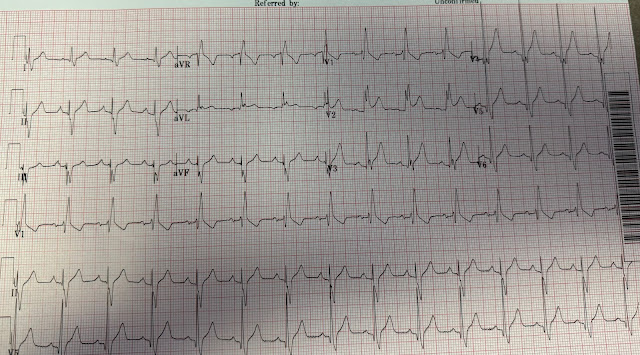
This ECG was texted to me by a colleague. I assumed it was from a patient with symptoms compatible with ACS/OMI.
There is sinus rhythm with RBBB and ST Elevation in V2 which is concordant with the QRS. The ST segment in RBBB should be ST depression, discordant to the positive R'-wave (i.e., opposite direction of the upright R'-wave) . But we sometimes see this concordant STE even in non-ischemic ECGs:
PseudoSTEMI and True ST elevation in Right Bundle Branch Block (RBBB). Don't miss case 4 at the bottom.
This STE suggests OMI, but we have seen many cases like this that are false positives (OMI mimics). I thought it did not look like OMI but was not willing to risk the patient's life by saying so.
I sent it to some EKG nerd friends (Pendell of course among them) and Pendell responded:
"So difficult. I’ll say real until proven otherwise. Baseline could invalidate that in 10 seconds."
Of course he is right. So I requested an old one.
And, of course, pretest probability is crucial, so I asked for the history: A 60 year old presented with palpitations and chest tightness.
In this case, if the patient needs PCI, he needs to be transferred because this hospital does not have a cath lab.
So getting the right diagnosis here is crucial.
I ran it by the Queen of Hearts PM Cardio app:
And then I got the Queen's explainability:
I relayed all our thoughts to my colleague.
The first troponin returned at 113 ng/L (elevated, but not by a lot). This is compatible with any kind of MI: type 1 (OMI or NOMI) or type 2. Or even with non-ischemic myocardial injury.
If you are convinced by all the data, including the troponin, that the patient's pain is due to ACS, and he has persistent pain, then he should go to the cath lab. But the clinician was not convinced and the ECG is not convincing.
That is to say, the troponin is not of definitive help.
Even if it were normal, it would not help: in 25% of proven occlusion, the first troponin is below the URL.
Wereski R, Chapman AR, Lee KK, Smith SW, Lowe DJ, Gray A, et al. High-Sensitivity Cardiac Troponin Concentrations at Presentation in Patients With ST-Segment Elevation Myocardial Infarction. JAMA Cardiol. novembro de 2020;5(11):1302–4.
Wanamaker BL, Seth MM, Sukul D, Dixon SR, Bhatt DL, Madder RD, et al. Relationship Between Troponin on Presentation and In-Hospital Mortality in Patients With ST-Segment-Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. J Am Heart Assoc. outubro de 2019;8(19):e013551.
The colleague looked harder for an old ECG and finally found one:
Further investigation revealed that the patient has a history of PSVT and that he probably was having a type 2 MI from an episode of prehospital PSVT.
He did not have OMI.
False positive ECGs are a source of frustration, and their frequency makes it harder to persuade interventionalists to take patients to the cath lab who have a subtle true positive. The old story of "Crying wolf" is a problem because when a wolf really is prowling, people won't believe you.
The Queen of Hearts PM Cardio AI app is amazing at differentiating ischemic ECGs from mimics. We believe it will result in far fewer false positive cath lab activations.
We are in the process of studying the Midwest STEMI Consoritium 20,000 cases of cath lab activation to see how well the Queen identifies false positives.
Stay tuned.
MY Comment, by KEN GRAUER, MD (11/1/2023):
===================================
- I was intrigued by this case — because it raises 2 Clinical Questions: i) Is this an acute OMI? (and should the cath lab be activated?) — and, ii) If not an acute OMI — What is likely to be going on?
-USE.png) |
| Figure-1: I've reproduced and labeled the initial ECG in today's case. (To improve visualization — I've digitized the original ECG using PMcardio). |
- The QRS complex is fragmented in multiple leads.
- Although the R wave in lead II is relatively tall (ie, ~6 mm) — QRS depolarization activity is predominantly negative in each of the 3 inferior leads — consistent with LAHB (Left Anterior HemiBlock). Therefore — there is bifascicular block (RBBB/LAHB).
- Small q waves are present in high-lateral leads I,aVL — and slightly larger q waves are seen in leads V3-thru-V6. While the lateral q waves look like benign septal q waves — it is much less common to see a q wave in lead V3, though the significance of this is uncertain.
- Fairly prominent R waves are seen in leads V4,5 — though not quite satisfying voltage criteria for LVH.
- My attention was immediately drawn to lead V2 — since the 2 mm of ST elevation seen in this lead looks like it could be acute. What makes the ST elevation in this lead worrisome — is that there is complete RBBB, with appropriate ST-T wave depression in lead V1.
- As noted by Dr. Smith — ST elevation should not normally be seen in lead V2 when there is complete RBBB and ST-T wave depression in lead V1. Instead — there is usually at least some ST-T wave depression in lead V2 (and usually also in lead V3) when there is complete RBBB.
- NOTE: It is not uncommon in patients who do not have OMI, but who manifest complete RBBB — to see some ST elevation in selected limb leads (especially in leads I and aVL — or in lead III) — and/or in lateral chest leads. That said — I do not recall having seen as a "benign variant" the type of acute-looking ST-T wave elevation that we see here in lead V2, in a patient with complete RBBB.
- NOTE: Other leads in Figure-1 also manifest some ST elevation (as highlighted by the dotted RED lines). That said — I would not have been concerned about the ST elevation in these other leads were it not for the ST-T wave appearance in lead V2.
- As I stated at the beginning of My Comment — Today's case raises 2 clinical questions: i) Is this an acute OMI? — and, ii) If not — What is likely to be going on? In my opinion — both of these questions need to be answered by the emergency provider.
- In today's case — We never learn the age, sex or history (beyond learning that the patient has had reentry SVT on one or more occasions in the past). Even if this patient does not have OMI — I would want to know this information to help figure out what might be going on.
- The presence of bifascicular block with fragmentation in multiple leads and the ECG findings described above — could indicate potentially significant underlying heart disease. At the least — I would want to know Echo findings regarding the presence (and potential severity) of any underlying heart disease.
- An initial troponin was elevated — albeit not be a lot.
- The "good news" = a prior ECG was found, which strongly suggested that none of the ST-T wave findings described above were acute. As a result — OMI in need of acute catheterization was felt to be safely ruled out!
- My Final Thoughts: I remain intellectually curious as to what may have been going on in today's patient. The potential is there for significant underlying heart disease (possibly with an entity such as recurrent myocarditis or something else that might need attention with additional measures for optimal management). That said — Today's 1st question as to whether or not to activate the cath lab can be answered with a NO.




No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.