This was sent by a colleague.
A 34 yo woman with a history of HTN, h/o SVT s/p ablation 2006, and 5 months post-partum presented with intermittent central chest pain and SOB.
She had one episode of pain the previous night and two additional episodes early on morning the morning she presented.
Deep breaths are painful and symptoms come and go. She had one BP that was measured at 160/120, uncertain when and what the BP was at other moments. Home meds were labetalol and nifedipine.
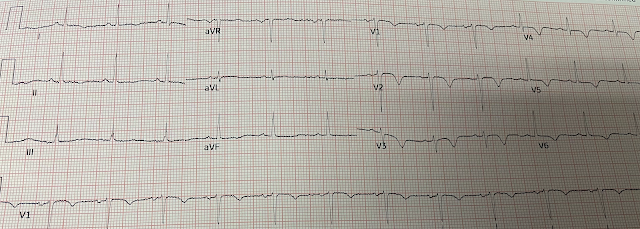
On the first ECG, the diagnosis of Wellens’ syndrome is not certain because:
1) the chest pain is pleuritic (not classic angina)
2) the BP is very high
3) The T-wave inversion morphology is non-specific (these are not typical Wellens' waves)
4) The patient is very low risk (a 34 year old with a HEART score of 2 and EDACS of (-2).
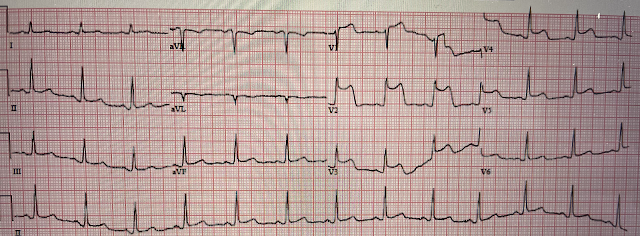
However, when there is evolution of the T-waves, as with the 2nd ECG, the specificity for Wellens' is much higher.
A repeat troponin returned at 0.45 ng/mL, consistent with reperfused OMI, or Non-OMI.
Now, with elevated troponins, Wellens' syndrome is likely.
A CT Coronary angiogram was ordered. Here are the results:
--Minimally obstructive coronary artery disease.
--LAD plaque with 0-25 percent stenosis. CAD-RADS category 1.
--No signs for aortic dissection or pulmonary embolus.
--"Results were discussed with the ordering physician. Given that the patient has had an abnormal elevated troponin, would suggest a Cardiology evaluation. Although a lesion is not visible anatomically on this CT scan, coronary catheter angiography could be considered based on Cardiology evaluation."
The patient was admitted.
Her echo was entirely normal.
Later, she developed chest pain again, and had this ECG recorded:
Coronary angiogram-
--Right dominant coronary artery system
--The left main artery was normal in appearance and free of obstructive disease.
--The LAD has moderate 40% ostial-proximal LAD stenosis and severe 90% mid LAD stenosis involving first diagonal branch.
--The circumflex artery was normal in appearance and free of obstructive disease.
--The ramus artery was normal in appearance and free of obstructive disease.
--The RCA was normal in appearance and free of obstructive disease.
INTERVENTION
* Successful angioplasty and stenting (drug eluting) of the mid LAD
* Successful angioplasty of the ostial 1st diagonal
Learning points:
1. Young women do get acute MI
2. Chest pain followed by a pain free period, with T-wave inversions in the LAD territory is likely to be Wellens' syndrome. It is much less likely if the ECG is recorded DURING pain.
3. Wellens' syndrome will almost always develop elevated troponins.
4. If there are T-wave inversions and elevated trops in the context of persistent pain, think of other pathologies such as pulmonary embolism.
5. Wellens' syndrome is a post-OMI syndrome after spontaneous reperfusion. It is likely that the artery will re-occlude. Thus, Wellens' syndrome should be thought of as a transient OMI or transient STEMI. Transient STEMI is at high risk of re-occlusion.
6. CT Coronary angiogram is usually used to make ACS much less likely in the context of a patient who is ruled out for acute MI by troponins. If trops are negative and there is <50% stenosis, then the patient is safe for discharge, even if the HEART score or EDACS score are elevated. Even with T-wave inversion, serial negative troponins all but rule out Wellens' syndrome. In this case, troponins were elevated and therefore the patient needs a conventional angiogram to look for a 1) a culprit, 2) stenosis that would account for type 2 MI, or 3) coronary dissection which is another possibility in a young woman.
7. There are other actual uses and potential uses of CTCA, but the above is the most common.
===================================
MY Comment, by KEN GRAUER, MD (5/10/2023):
===================================
- For clarity in Figure-1 — I've reproduced the first 2 tracings in today's case.
-USE.png) |
| Figure-1: The first 2 ECGs in today's case. (To improve visualization — I've digitized the original ECG using PMcardio). |
- Despite the young age of this woman — and despite her lack of CP (Chest Pain) at the time she presented to the ED — the treating clinicians were appropriately concerned about her initial ECG (and her slight-but-significant initial troponin elevation). This led to further evaluation with a repeat ECG, a repeat troponin, CTCA (CT Coronary Angiogram), and Echo.
- Cardiology On-Call was consulted by emergency providers for consideration of cardiac cath — despite no more than minimal disease on CTCA.
- A 3rd ECG was promptly recorded when this patient's CP recurred — and this 3rd ECG showed an obvious STEMI that made the decision for prompt cardiac cath easy!
- It is with this goal in mind that I'll retrace my sequential thoughts on learning about this case.
- Nonspecific ST-T wave flattening is seen in the limb leads.
- The most remarkable finding on ECG #1 — is fairly shallow but-definitely-present T wave inversion in leads V1-thru-V5. I found it of interest (albeit a bit confusing) — the fact that there was definite coving of the ST segment in lead V2, with deeper T wave inversion than in lead V3 — but with increased T wave inversion returning in lead V4.
- Bottom Line about ECG #1: I thought this initial ECG was non-diagnostic.
- Given the above symptoms (that apparently were severe enough to prompt her presentation to the ED) — and given the principal finding of her non-diagnostic initial ECG (ie, no more than modest T wave inversion — but which was present in multiple chest leads — with verbal report that such T wave inversion was not previously present) — I contemplated 3 possible etiologies for the findings in ECG #1:
- Possibility #1: T wave inversion in the chest leads, especially in association with dyspnea and "painful breathing" — could be the result of pulmonary embolism. That said, against acute PE — is the inconstancy of this patient's symptoms — the lack of tachycardia — and the lack of any other ECG signs of acute RV strain.
- Possibility #2: As per Dr. Smith's discussion — the modest chest lead T wave inversion in ECG #1 could reflect Wellens' Syndrome (ie, reperfusion T waves following brief coronary occlusion) — especially given slight-but-real troponin elevation in this patient whose CP had resolved at the time this initial ECG was recorded.
- Possibility #3: This initial ECG is non-diagnostic — and may be unrelated to this patient's symptoms. Over the years — I've learned "the hard way" that no matter how capable a colleague may be — verbal or written report of prior ECG findings without the actual ECG for me to review with my own eyes, may or may not truly show what has been reported. There are non-cardiac and non-pulmonary potential causes of shallow T wave inversion not unlike what we see in ECG #1 — and this patient's description of symptoms is not clearly suggestive of any acute cardio-pulmonary cause.
- So — as per the superb teaching point made by Dr. Smith — we can not tell for certain if the troponin elevation with deepening T wave inversion seen in all 6 chest leads of ECG #2 is the result of: i) Evolving Wellens' Syndrome; or, ii) Non-OMI due to supply-demand mismatch.
- Clinically — this does not matter, because dynamic ST-T wave changes on serial tracings in a patient with intermittent chest pain and troponin elevation is indication to establish the diagnosis (and to perform PCI if/as clinicated indicated by diagnostic cath).
- Was a purpose served by obtaining CTCA? A purpose would be served — if a negative CTCA would make an acute coronary syndrome unlikely enough as to obviate the need for cath. But this patient with intermittent CP already had positive troponin and dynamic ECG changes on repeat ECG — such that regardless of the "non-obstructive coronary disease" on CTCA — conventional cath is needed. As a learning point — there is no need to delay cath by ordering a CTCA that will not change the need for cath.
- How long did providers wait to repeat the initial ECG?
- Was the patient having symptoms at the time ECG #2 was obtained?
- For example — IF ECG #1 represents the initial stage of developing reperfusion associated with evolving Wellens' Syndrome — then we might soon (within the next 15-to-40 minutes, or so) see an ECG similar to the appearance in ECG #2, in the continued absence of chest pain.
- If on the other hand — several hours passed until ECG #2 was obtained, at which time the patient was having increased CP — we might be led to a different conclusion.


No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.