Submitted and written by Megan Lieb, DO with edits by Bracey, Smith, Meyers, and Grauer
A 50-ish year old man with ICD presented to the emergency department with substernal chest pain for 3 hours prior to arrival. The screening physician ordered an EKG and noted his ashen appearance and moderate distress.
Triage EKG:
 |
| What do you think? |
Triage physician interpretation:
-sinus bradycardia
-lateral ST depressions
While there are lateral ST depressions (V5, V6) the deepest ST depressions are in V4. Additionally, lead V3 has ST depressions, which are always abnormal (recall that lead V3 will have ST elevation under normal circumstances!)
Smith: also VERY important is the downsloping ST segment in V3. This is a very specific marker of posterior OMI. Additionally, V2 has a very flattened T-wave, which is typical of posterior OMI.
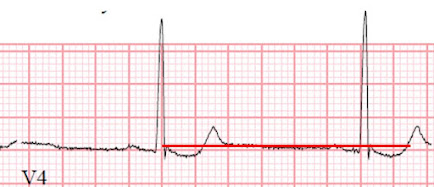 |
| Close up of V4 with baseline in red |
This ECG alone is highly suspicious for posterior OMI! This pattern is recognizable by the ST depressions maximal in lead V4. Recall that, in the setting of ACS symptoms, ST depression that are maximal in leads V1-V4 (as opposed to V5 and V6) not attributable to an abnormal QRS complex is specific for OMI.
 |
| ST depression markedly worse in V3 and V4 |
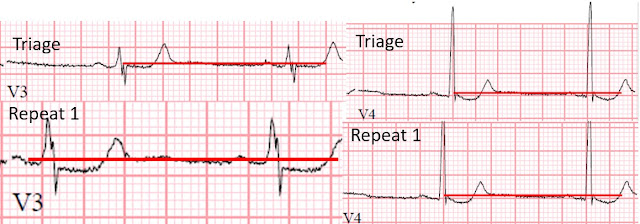 |
| Comparison of leads V3 and V4 |
While the ICD was preparing to be interrogated, the interventional cardiologist was consulted for evaluation for emergency catheterization. After reviewing the available information, cardiology did not feel that the patient warranted emergent PCI and recommended heparin infusion and cardiac catheterization the following morning.
Around this time the troponin I resulted at 0.05 ng/mL (ULN 0.04).
A second ECG was performed this time:
 |
| Resolution of ST depression in the anterolateral leads |
A posterior ECG was also performed at this time:
The cardiology service was alerted to the finding of episodes of VF and obvious dynamic ECG changes and did not feel immediate cath was indicated, and instead deferred cardiac cath until the next morning.
A repeat troponin I was elevated at 0.07 ng/mL and 7.59 ng/mL at hours 4 and 7 from arrival respectively. Serum troponin I level just before the cardiac catheterization procedure was 16.69 ng/mL.
 |
| 90% stenosis of the proximal ramus intermedius, pre procedure TIMI II flow |
The ramus intermedius is a normal variant on coronary anatomy that arises between the LAD and LCX. Its course is variable, often supplying the lateral wall of the LV. In this case, the vessel supplied a portion of the posterior LV circulation.
 |
| Post procedure 0% stenosis, TIMI III flow |
A post procedure ECG was performed 24 hours after PCI:
 |
| Standard orientation 12-lead ECG demonstrating reperfusion of infarcted territory |
Note that leads V2-4 show posterior reperfusion T waves (now more upright in these leads, as they are reciprocal to negative, reperfusion T waves inversions on posterior leads). Lead aVL also demonstrates typical reperfusion pattern, indicating high lateral wall reperfusion.
 |
The patient was started on dual antiplatelet therapy and discharged from the hospital on day 3 without further event.
Take home points:
ST depressions maximal in leads V1-V4 (not otherwise attributable to an abnormal QRS complex) are highly specific for posterior OMI in a patient with new ischemic symptoms.
Serial ECGs are often helpful in identifying more subtle ECG manifestations of OMI
Posterior leads will often have little to no ST elevation even in the setting of posterior OMI owing to lung tissue being in between the posterior LV wall and the posterior chest wall. However, when the ST depressions resolve, there will be no ST elevations in posterior leads either, as this case highlights. Recall that air is a poor conductor of electricity and will, therefore, generate smaller amplitudes on posterior leads (hence why STEMI criteria requires only >0.5 mm in any posterior lead to be considered positive). Thus, it is essential for you to be able to recognize posterior OMI in the standard orientation 12-lead ECG!
Ventricular fibrillation is a common outcome in OMI and should greatly heighten the suspicion for ischemic heart disease even in the absence of profound ST elevation.
- Given the history of new-onset chest pain and this patient's initial appearance described as "ashen and in moderate distress" — the cath lab should have been activated immediately on seeing ECG #1.
-USE%20copy.png) |
| Figure-1: The initial ECG in today's case. I've added a magnified view of the mirror-image of the 1st complex in lead V3 (within the RED-border insert). |
- The "similar situations" I was referring to in my opening sentence — relates to 3 Oversights made by all-too-many clinicians. These oversights are: i) Failure to appreciate the characteristic "shape" of ST-T wave depression in the anterior chest leads, that when seen in a patient with new chest pain is indicative of acute posterior OMI; ii) Failure to appreciate that the "culprit" artery in many acute occlusion MIs will spontaneously reopen (thereby reperfusing) even without treatment — sometimes opening, then reclosing, then reopening again a number of times until eventually the vessel's final state is reached; and, iii) Even without ST elevation — a patient with new-onset and persistent cardiac chest pain that occurs in association with ischemic ST depression is indication for prompt cath.
- I don't know why the pattern of ST-T wave abnormality seen in lead V3 of ECG #1 continues to go unrecognized by all-too-many clinicians. I've found the easiest way to convey appreciation for this important ECG sign — is with the Mirror Test. As I've illustrated multiple times in Dr. Smith's ECG Blog, the Mirror Test is simply a visual aid that facilitates recognition of acute posterior OMI from the standard 12-lead ECG without need to apply posterior leads (See My Comment at the bottom of the page in the September 21, 2022 post).
- The rationale for the Mirror Test is based on the premise that anterior leads provide a mirror image of electrical activity in the posterior wall of the left ventricle. By simply inverting a standard 12-lead ECG, and then holding it up to the light — you can easily visualize the "mirror-image" of leads V1-thru-V4.
- In Figure-1 — the principal lead showing a positive Mirror Test is lead V3 (Seen within the magnified, RED-border mirror-image insert of lead V3). QUESTION: Doesn't the shape of the slightly elevated ST segment, in association with deep, symmetric T wave inversion in this lead suggest acute infarction?
- As suggested in Figure-1 by the deep T wave inversion within the RED-border insert — the peaked T wave in lead V3 strongly suggests that there has been at least some reperfusion of the "culprit" artery. That this might happen should not be surprising — since the patient's chest pain was already ongoing for 3 hours prior to arrival in the ED.
- Additional evidence in support of spontaneous "culprit" artery reperfusion in ECG #1 — is suggested by the flat ST segment in neighboring lead V2. With acute posterior OMI — ST depression is typically most marked in leads V2,V3,V4 — such that the flat ST segment in lead V2 presumably reflects some return-to-the-baseline of the ST depression that most probably had been present earlier in lead V2.
- Final evidence in strong support of recurrent spontaneous opening and reclosure of the "culprit" artery — was forthcoming when the patient revealed having several syncopal episodes while at home during the previous 24 hours, with each episode culminating in a shock from his implanted ICD.
- The patient's "ashen appearance" with ongoing chest pain at the time he arrived in the ED — in association with the diffuse ST segment changes on the initial ECG — should have been enough to indicate prompt cath, even without recognizing that the ST-T wave appearance in lead V3 of ECG #1 was diagnostic of acute posterior OMI.
- If doubt remained about the need for cath after reviewing the initial ECG — the recent history of 2 syncopal epsiodes that were both terminated by ICD shock — and/or — the subsequent dynamic ST-T wave changes on serial ECGs would have more than satisfied criteria for prompt cath.




No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.