Thanks to our Electrophysiologists Omar Iqbal and Rehan Karim for the below strips and the explanations I will be giving on this post.
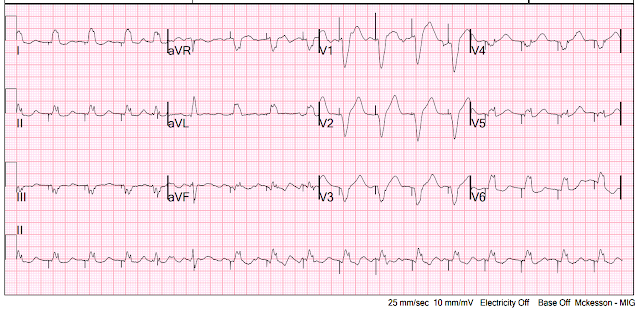
A patient had 3rd degree AV block in the ED. A transvenous pacer was placed in the Emergency Department by the emergency physicians. Capture was obtained and a 12-lead ECG was recorded:
The 5th beat (the one with the 4th visible pacer spike) comes early (PAC or PVC), and the pacing spike occurs AFTER initiation of the QRS. (Ken Grauer points out that this 5th beat appears to be due to an early atrial beat and that these early beats continue for a few beats, suggesting a short run of atrial tachycardia.)
The 6th beat (the one with the 5th visible pacer spike) has a pacing spike in the midst of the QRS.
What does it mean that the pacing spike comes in the midst of the 5th and 6th native beats?
This means that the pacer is either failing to "sense" the native beats (usually due to less-than-perfect placement) or that it is on "asynchronous" mode in which it will fire regardless of the native beats (it is set so that even if it senses the native beat, it will pace regardless).
Asynchronous pacing seems like the safe setting, EXCEPT that it means that the pacemaker can trigger on the T-wave, which can result in Ventricular Fibrillation.
Our electrophysiologists give an example of this here:
"Asynchronous" mode means that the pacemaker will pace regardless of what the native beats are doing. Thus, it can pace on the T-wave, as above.
But this can also happen in "demand" mode if the pacer fails to sense.
Demand mode is when the pacer is sensing. If it senses a native beat, it will not pace unless another native beat is not sensed within a specific time period. For instance, if the rate is set at 60 beats per minute in demand pacing, it will wait 1 second before pacing. If it senses a beat in under 1 second, it will not pace. If it does not sense a beat, it will pace.
Usually, failure to sense is due to poor placement, and the pacer may also fail to pace in such a situation.
However, it is possible that the pacer can fail to sense even though it can pace. In such a situation, there can also be the dangerous pacing on a T-wave.
The pacer in the strip below was NOT in aysnchronous mode; it is in demand mode. It simply was failing to sense even though it could pace:
All pacing spikes except #6 here are inappropriate; all others should have been inhibited. #6 does wait a full second before firing, but it is waiting a second after a paced beat; it appears that the appropriate delay is ONLY because there is no intervening native beat which it would otherwise fail to sense!
It is failing to sense all native beats (Beats 1, 2, 4, 5, 7, 10, 12, 14)
Beat #9 (pacing spike #6) occurs simultaneous with the spike, and therefore looks like a native beat.
Beats 3, 6, 8, 11, 13 are paced.
There are 8 Pacing spikes: numbers 2, 4, 5, 7, and 8 capture
Pacing spikes 1, 3 do not capture because they are in the midst of the QRST. The 3rd pacing spike comes directly on the T-wave (though not on the latter part of it)!
- Dr. Smith asked the question of what complication might arise from what you see in Figure-1?
-USE.png) |
| Figure-1: What do you see? What complication might arise? |
- To Emphasize — There clearly are times when a pacemaker will malfunction. The pacemaker is not always "right". But when all but a small segment of a long lead recording shows appropriate sensing and capture — there may be a physiologic (and beneficial) reason for that small rhythm segment that is confusing me.
- Beat #5 comes early. Instead of being preceded by a pacing spike (as seen for paced beats #2,3,4) — an on-time pacing spike occurs in the middle of beat #5. Why does this happen? If the pacer was set on Demand Mode — then shouldn't the pacer have been inhibited by slightly-early-occurring beat #5?
- Clearly — it is difficult to identify atrial activity throughout most of the long lead II rhythm strip in Figure-1 (due to a combination of artifact and the late-occurring T wave of paced beats). That said — I believe the equally-spaced RED arrows highlight 7 consecutive atrial deflections from a short run of either ATach or AFlutter.
- Trying to understand "HOW the pacemaker may be right" — I thought it reasonable to postulate that the reason beat #5 occurs earlier-than-expected — is that the 1st atrial beat in this run ( = the 1st RED arrow) conducts!
- Rather than postulating pacemaker malfunction — the 4th pacemaker spike (that occurs in the middle of the 5th QRS complex) — may simply not have had enough time to be inhibited. The result is that beat #5 is a fusion beat, manifesting a QRS morphology with features intermediate between spontaneous conduction and paced beats.
- The QRS of beat #6 also looks different than paced beats. Once again — the 5th pacer spike falls in the middle of this 6th QRS complex at the same 100/minute pacing rate maintained throughout this tracing. Note how QRS morphology of beat #6 looks even more different from paced beats than did beat #5! (This is best seen by comparing QRS morphology of beat #6 in simultaneously-recorded leads aVR,aVL,aVF to the paced beats in these leads). Beat #6 is a fusion beat. The reason that it also occurs slightly earlier-than-expected — is that it too appears to be conducted (by either the 3rd or 4th RED arrow P wave).
- I believe the run of ATach (or AFlutter) ends after the 7th RED arrow — after which to continually on-time pacer spikes regain regular capture at 100/minute.
- BOTTOM Line: Although faulty sensing or use of asynchronous mode are potential reasons why pacer spikes may unexpectedly appear in the middle of QRS complexes — I do not think that is occurring here. Instead — I suspect the underlying rhythm changed for a short run of ATach (or AFlutter). Spontaneous conduction of atrial impulses late in the cycle might account for why the 4th and 5th pacer spikes in today's example occur in the middle of QRS complexes. I do not think the pacemaker was "wrong". Instead — I simply don't think the pacer had an adequate chance to be inhibited.
- For those wanting more on Pacing — I like the PDF review of Pacing Basics by the University of Ottawa Heart Institute — and the user-friendly summary of Temporary Pacemaker Troubleshooting in the November 3, 2020 Life-In-The-Fast-Lane. — and the 2021 YouTube Review by ICU Advantage on "Temporary Pacemakers: Modes and Basic Settings".

.PNG)
.png)
No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.