A young man suffered multiple gunshot wounds. He complained of worsening dyspnea en route to the emergency department and was placed on nonrebreather facemask. On initial exam he had penetrating wounds to the left chest with a rigid abdomen and superficial wounds to the lower extremities. E-FAST examination showed bilateral lung sliding with a small pericardial effusion without evidence of tamponade. He was taken emergently to the operating room where he underwent exploratory laparotomy with subxiphoid pericardial window, median sternotomy, and repair of penetrating cardiac injury to the apex of the left ventricle along with repair of multiple intraabdominal injuries.
Here is part of his operative report:
"There was a left central diaphragmatic injury with ongoing bleeding consistent with decompressing hemopericardium. Subxiphoid pericardial window was performed confirming hemopericardium. Thus median sternotomy was performed. Hemopericardium was evacuated. Heart was examined with note of a penetrating injury to the apex of the left ventricle. There was moderate surrounding contusion and active bleeding. Given injury pattern and location, primary repair with sutures was performed. A total of 2 horizontal mattress pledgeted sutures were placed. There was no apparent involvement of the cardiac vessels."
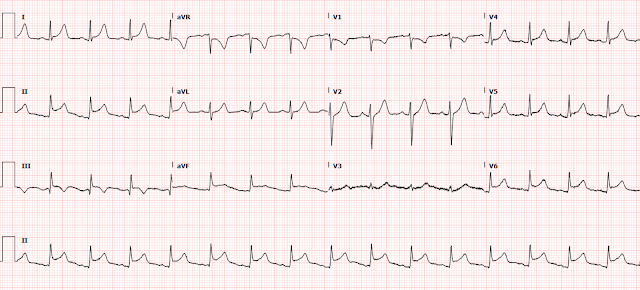
On hospital day 1, the following EKG was obtained:
What do you think? What diagnoses should be on the differential given the known injury pattern?
There is frank ST elevation in multiple leads (V4-6, I, II, III, aVF) with reciprocal STD in aVR and V1. Some leads have accompanying large T waves suspicious for hyperacute T waves, while others like lead aVF have a distinct appearance of STE without large T waves (in pericarditis we sometimes discuss the ST / T ratio, as classic OMI typically has large T waves and large STE, while pericarditis sometimes has relatively small T waves compared to the STE).
The down-sloping TP segment is referred to as Spodick's sign, and is most obvious in lead II.
A transthoracic echocardiogram was obtained which showed an LVEF of 55-60% with a trivial pericardial effusion. There was no evidence of tamponade or appreciable wall motion abnormality. The patient was treated with Toradol for his chest pain (presumably giving NSAIDs for anti-inflammatory action against pericarditis) and endorsed significant pain reduction.
The following EKG was obtained after 5 days and showed normalization of the patient’s ST abnormalities.
The two ECGs above were the only ones ever performed during his hospitalization.
In addition to his traumatic injuries, this patient was ultimately diagnosed with traumatic uncomplicated pericarditis. He was eventually discharged from the hospital in stable condition. There has not been any available follow up information for this patient.
On hospital day 1, the following EKG was obtained:
What do you think? What diagnoses should be on the differential given the known injury pattern?
There is frank ST elevation in multiple leads (V4-6, I, II, III, aVF) with reciprocal STD in aVR and V1. Some leads have accompanying large T waves suspicious for hyperacute T waves, while others like lead aVF have a distinct appearance of STE without large T waves (in pericarditis we sometimes discuss the ST / T ratio, as classic OMI typically has large T waves and large STE, while pericarditis sometimes has relatively small T waves compared to the STE).
Given the known gunshot wound to the heart, the differential could include: direct injury/occlusion of an epicardial coronary artery (such as the LAD) causing MI (including traumatic dissection), direct tissue trauma causing injury current manifesting as STE, or some kind of myopericarditis as a result of the injury, or multiple of these etiologies in combination.
The apex of the LV is most often supplied by the LAD, and OMI including the apex can sometimes cause confusion about the associated ECG leads. The most common and important pitfall is: large LAD occlusion often includes apical AMI, which can manifest OMI ECG findings in the "inferior" and/or "lateral" leads due to the relatively inferior and lateral position of the apex. The pitfall is that some providers will mistakenly believe that this pattern indicates "diffuse" STE, which makes them think more of pericarditis because classic ECG teaching advises that diffuse STE is indicative of pericarditis.
The down-sloping TP segment is referred to as Spodick's sign, and is most obvious in lead II.
In this study of Spodick sign and other potential discriminators between OMI and pericarditis, Spodick sign was noted (by a single expert, Dr. Mattu) in 5% of "STEMI" patients and 29% of "pericarditis" patients.
A transthoracic echocardiogram was obtained which showed an LVEF of 55-60% with a trivial pericardial effusion. There was no evidence of tamponade or appreciable wall motion abnormality. The patient was treated with Toradol for his chest pain (presumably giving NSAIDs for anti-inflammatory action against pericarditis) and endorsed significant pain reduction.
No cath or CT angiogram was ever done.
No troponin was ever ordered.
He underwent treatment of multiple traumatic injuries.
The following EKG was obtained after 5 days and showed normalization of the patient’s ST abnormalities.
The two ECGs above were the only ones ever performed during his hospitalization.
In addition to his traumatic injuries, this patient was ultimately diagnosed with traumatic uncomplicated pericarditis. He was eventually discharged from the hospital in stable condition. There has not been any available follow up information for this patient.
Learning Points:
This patient probably did not have acute coronary occlusion, but the workup performed would have been insufficient to detect acute coronary occlusion if he had suffered it. But they had direct visualization of the injured myocardium, which may also have high accuracy for ruling out coronary occlusion!
Traumatic injuries can cause direct damage to coronary arteries resulting thrombotic occlusion or dissection, which then causes OMI just like any other cause of acute coronary occlusion.
The only way to definitively rule out coronary occlusion in cases like this is angiography (perhaps in the future CT coronary angiogram could be perfect for this situation). MRI is good if you are not in a hurry, such as this case.
ECG changes of the apical myocardium may appear in the lateral leads V5-6 and inferior leads II, III, aVF.
Anytime there is a finding in multiple left sided leads, the opposite finding must be present in lead aVR.
===================================
Comment by KEN GRAUER, MD (6/8/2022):
===================================
The young man in today's case was lucky to have survived multiple gunshot wounds — including a penetrating wound to the heart. In addition to his traumatic injuries — he was discharged from the hospital with a diagnosis of traumatic uncomplicated pericarditis. Realizing that the circumstances of today's case are very different from the usual setting that prompts consideration of a diagnosis of acute pericarditis — I still thought the topic of the ECG Diagnosis of Acute Pericarditis to be a worthy one for our periodic review.
- I found it difficult to locate literature on specific ECG findings with traumatic pericarditis from penetrating cardiac trauma. As alluded to in the above discussion by Drs. Nicholson and Meyers — you might find almost anything on ECG, depending on the specific nature of cardiac injury (ie, there may be direct damage to coronary arteries resulting in acute thrombotic occlusion or dissection — pericardial effusion, possibly with tamponade — pneumopericardium — neighboring pneumothorax, including tension pneumothorax altering the relationship of anatomic structures — and/or cardiac contusion of varying severity).
- In contrast — a specific set of ECG findings has been described for non-traumatic acute pericarditis (See below). By way of perspective — despite being one of the most common considerations in international ECG forums — acute pericarditis is extremely uncommon in clinical practice.
- As has been emphasized many times on Dr. Smith’s ECG Blog — acute pericarditis is far less common than acute MI or a repolarization variant among patients who present to an emergency setting. As per Dr. Smith, “You diagnose acute pericarditis at your peril!" That said — it is good to keep in mind what the ECG criteria for this diagnosis are.
The Initial ECG in Today's Case:
For clarity — I've reproduced in Figure-1 the initial ECG in today's case. From a purely educational perspective — I thought it interesting to assess this initial ECG for findings consistent with a diagnosis of acute pericarditis — as well as for findings against that diagnosis.
-USE%20copy.png) |
| Figure-1: The initial ECG in today's case. |
ANSWERS:
- ECG findings in Figure-1 consistent with acute pericarditis include: i) Upward sloping ST elevation in multiple leads; ii) Spodick's sign (most obvious in lead II — as per Drs. Nicholson and Meyers); and, iii) The ST-T wave ratio in lead V6 is >0.25 (whereas it tends to be less than this with repolarization variants).
- Of no diagnostic help in Figure-1 is the finding of PR depression — which is seen in some but not other leads (ie, it is present in leads II, V4,5,6). Even if PR depression was more diffuse — the specificity of this finding for acute pericarditis is modest at best.
- ECG findings in Figure-1 against the diagnosis of acute pericarditis include: i) There is a fairly large Q wave with ST elevation and T wave inversion in lead III that resembles the picture of acute MI (whereas with acute pericarditis — Q waves should not be seen — and T wave inversion typically does not begin until ST elevation has resolved); and, ii) ST elevation is lacking in leads aVL, V2 and V3 (The ST segment straightening in leads aVL and V3 is much more characteristic of coronary disease than acute pericarditis).
Conclusion: The ECG in Figure-1 would not be typical for non-traumatic acute pericarditis. However, it could be consistent with traumatic pericarditis (because ECG findings are so variable in traumatic pericarditis).
- NOTE: The ECG features of acute myocarditis may differ substantially from those of a "pure" pericarditis. There may be a resemblance between these 2 entities — but ST segment deviations (elevation and depression) with myocarditis may not follow the timing seen with pericarditis. In addition, Q waves may develop — so at times it may be difficult to distinguish myocarditis from infarction on ECG.
=====================
ECG Findings of Acute Pericarditis:
By way of Review — I’ve excerpted in Figure-2, relevant paragraphs from a 2017 ESC (European Society of Cardiology) article on this subject by Xanthopoulos & Skoularigis (ESC: Vol. 15, No.15-9/6/2017).
- CLICK HERE — for a 9-page PDF of "My Take" on the ECG diagnosis of acute pericarditis.
Among the KEY points regarding ECG diagnosis of acute pericarditis from Figure-2 (to which I’ve added some of my own points) — are the following:
- Typical ECG findings of acute pericarditis are not always present! The ECG is far from a perfect diagnostic tool.
- 4 Stages are described in the ECG evolution of Acute Pericarditis findings. These can be summarized as: i) Stage I — in which there is generalized ST elevation in most leads (except perhaps in the “right-sided” leads = leads III, aVR and V1); ii) Stage II — in which this generalized ST elevation returns to baseline (ie, “pseudo-normalization” phase); iii) Stage III — in which there is diffuse T wave inversion; and, iv) Stage IV — in which the overall tracing normalizes.
- Of these 4 stages — only Stage I is readily recognizable as potentially due to acute pericarditis. You would never guess “pericarditis” if given an isolated tracing from Stage II, III or IV.
- The time course of these 4 ECG Stages (in those pericarditis cases in which they occur) — is highly variable. The ESC summary in Figure-2 states that Stage I may last “between hours to days” — before evolving into Stage II.
- The shape of the ST elevation is typically concave-up (ie, a “smiley” configuration).
- ECG signs usually associated with acute MI (ie, abnormally large or wide Q waves — reciprocal ST depression) are absent!
- PEARL: The appearance of the ST-T wave in lead II tends to resemble that in lead I with acute pericarditis. In contrast, with acute MI — ST-T wave appearance in lead II resembles lead III (and not lead I).
- There may be PR depression in many leads — with “reciprocal” PR elevation in lead aVR.
- The RATIO of the amount of ST elevation to T wave amplitude in lead V6 should be more than 0.25 (ie, height of the ST elevation, as measured from the end of the PR segment to the J-point — should be more than 1/4 of the height of the T wave in lead V6 — as shown below in Figure-3).
-USE%20copy.png) |
| Figure-3: Illustration of how the ST segment to T wave ratio is calculated — adapted from Life-In-The-Fast-Lane (and taken from My Comment in the December 13, 2019 post of Dr. Smith's ECG Blog). |




-USE.png)
No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.