This was texted to me from 2000 miles away. It is from a 30-something male with chest pain.
There was worry for ischemia.
No. There is not. All of the ST-T abnormalities are secondary to the abnormal QRS that is produced by pre-excitation. This is WPW.
Notice the very short PR interval. Notice the obvious delta waves.
Most, but not all, of the ST elevation and ST depression are discordant to the abnormal QRS, and are not excessively discordant.
In contrast, in the ECG below, the discordant ST elevation and ST depression are out of proportion to the QRS (which is abnormal due to WPW, with delta waves):
See a number of other WPW cases here:
===================================
MY Comment by KEN GRAUER, MD (4/5/2022):
===================================
Today's case provides an excellent example of why WPW is so often referred to as, "the great ECG mimic". This is because of the multitude of entities that this ECG abnormality may resemble including:
- LVH (with a "strain"-like pattern in lateral leads).
- RVH (with a predominant R wave in lead V1 from a left-sided accessory pathway).
- RBBB or LBBB (from QRS widening plus morphology that closely resembles these conduction defects).
- Myocardial ischemia and/or infarction (negative delta waves may simulate Q waves — and ST-T wave abnormalities associated with WPW may closely resemble those of ischemia or infarction).
As a result of this close resemblance to other ECG entities — most of the time (in my experience) — once preexcitation with WPW is recognized, it is difficult (if not impossible) to say much more about the tracing. The 2nd tracing shown above by Dr. Smith demonstrates a notable exception to this generality — in which despite the presence of WPW, a superimposed acute infero-postero MI is present and diagnosable on ECG! The lesson conveyed by this example from Dr. Smith is clear:
- Sometimes you can diagnose acute coronary occlusion by ECG in a patient with underlying WPW!
While keeping this important lesson conveyed by Dr. Smith in mind — I wanted to put forth the corollary of this situation — namely that — sometimes with WPW, even though the ECG "looks like" acute coronary occlusion — the ST-T wave abnormalities you see may simply be the result of WPW.
- Bottom Line: Sometimes in a patient with WPW, who presents with chest pain — you simply will not be able to tell from the ECG if there is (or is not) acute coronary occlusion.
The ECG in Figure-1 is from a 35-year old man who presented with new-onset chest pain. What do YOU think?
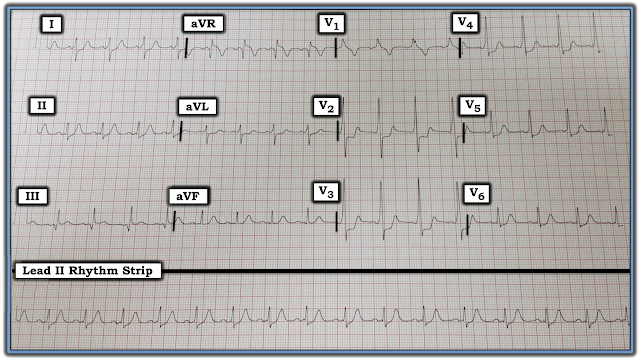 |
| Figure-1: ECG obtained from a 35-year old man with chest pain (I originally published this case HERE). |
My Thoughts on this Tracing:
The rhythm in Figure-1 is sinus at a rate of ~90/minute. Although at first glance (ie, looking at lead II) — the PR interval looks to be normal — the QRS is wide, delta waves are present in certain leads and the PR interval is short in those leads with delta waves (See RED arrows in Figure-2). This patient has WPW.
- PEARL #1: Delta waves are not always seen in all 12 leads of the ECG when a patient has WPW. As a result, it can sometimes be quite challenging to make the diagnosis. This problem is complicated by the reality that some patients (more common in older individuals) normally manifest some initial slowing (and therefore slurring) of the early part of the QRS complex. Therefore: When contemplating the possibility of WPW — all 12 leads should be carefully scrutinized. If questionable initial slurring is minimal and only noted in 1 or 2 leads — then the patient probably does not have WPW. But if unmistakable delta waves associated with a short PR interval are definitely seen (as highlighted by the RED arrows in leads V2, V3 and V4 of Figure-2) — then you have made your diagnosis despite the absence of obvious delta waves in some of the other leads.
- PEARL #2: Once you determine the patient has WPW — you’ll often be able to GO BACK and recognize subtle deflections that in retrospect are also delta waves. For example, in Figure-2 — I initially thought there was a Q wave in lead III (WHITE arrow). However, the fact that this negative deflection in lead III occurs at precisely the same instant in time as the delta wave in simultaneously-obtained lead I (dotted WHITE line, leading up to the RED arrow in lead I) — tells us that this negative deflection in lead III is actually a negative delta wave.
- Other examples of “retrospective recognition” of delta waves in Figure-2 are seen in leads II, aVL, and aVF. Thus, the suggestion of a tiny “extra little bump” on the baseline in leads II and aVF probably represents subtle delta waves that are almost entirely isoelectric.
 |
| Figure-2: I have labeled the ECG in Figure-1 to illustrate subtle delta waves. But what about the ST depression within the WHITE rectangles? |
=============================
As noted — the patient whose ECG is shown in Figure-2 was a 35-year old man who presented with new-onset chest pain.
- What about the "shelf-like" ST depression seen within the WHITE rectangles? This worrisome-looking ST depression is maximal in leads V2-thru-V4 — which in a patient with new chest pain, we've been taught to reflexively consider acute posterior OMI.
Follow-Up to this CASE:
The cardiologist involved in this case was as uncertain as I was looking at this ST depression (within the WHITE rectangles) — as to whether this reflected acute coronary occlusion — or was simply an accompaniment of this patient’s WPW.
- Cardiac cath was performed. It turned out that the coronary arteries were free of significant disease.
LESSON: Much (if not most) of the time — you will not be able to appreciate ischemia or acute infarction on the ECG of a patient with WPW. That said, on occasion — ST-T wave changes may be prominent enough to suggest acute disease. In such cases — cardiac cath may be needed to define the anatomy. This was the situation in the case I presented.



No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.