Case sent by Magnus Nossen MD, edits by Meyers
A previously healthy woman in her 60s presented to an outpatient clinic for palpitations. Vitals were within normal limits other than heart rate. The ECG there reportedly showed an irregular tachycardia, and the patient was immediately referred to the emergency room.
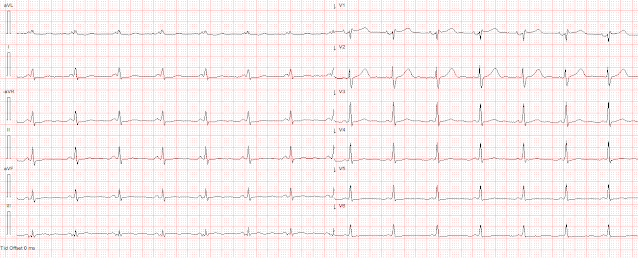
Here is her ECG on arrival:
There is a wide complex tachycardia that is irregularly irregular (this is difficult to determine at these very high rates). The QRS morphology appears almost monomorphic in some places, and polymorphic in others. The rhythm differential could conceivably include PMVT, stopping/starting VT, AF with WPW, AF with aberrancy, or an SVT with aberrancy that is stopping/starting.
In my opinion, it is too organized for classic PMVT.
Because it is irregularly irregular and polymorphic, I would assume it is AF with WPW until proven otherwise, but in my experience this ECG demonstrates a relatively low level of QRS polymorphism and it is less irregular than most AF WPW.
Both irregular and polymorphic QRS rhythms are contraindications to adenosine.
Procainamide would be a good choice, and electricity is always a good choice.
She was sedated and cardioverted.
Here is her post-cardioversion ECG:
ECG#2 - Immediately post cardioversion: Appropriate ST depression maximal in V5-6 and lead II, secondary to subendocardial ischemia, likely residual from the preceding tachycardia. There is a short PR interval and subtle delta waves in many leads.
She remained asymptomatic. She was admitted for further workup.
Telemetry caught this event:
This appears to show a paroxysmal atrial tachycardia which conducts, resulting in a wide complex tachycardia. Lead aVR seems to show the atrial activity clearly. There is some mild QRS polymorphism.
Here is her ECG the next day:
ECG following day with more apparent pre-excitation.
Echocardiography was normal.
Patient was referred to electrophysiologic testing due to suspicion of afib and WPW. During electrophysiologic testing AVRT was induced, which degenerated to afib with ortho and antidromic conduction. Radiofrequency ablation was performed for a right sided posteroseptal bypass tract.
Learning Points:
Irregularly irregular wide complex tachycardias include PMVT, AF with aberrancy (BBB, NSIVCD, etc), and AF with WPW.
Important features of AF with WPW include polymorphic QRS complexes and very short R-R intervals (as short as 200 msec or even less), corresponding to very rapid ventricular rates.
Options for AF with WPW include procainamide and cardioversion.
Other cases involving AF with WPW:
A 47-year-old man with abdominal pain and heart rates approaching 300 bpm
Here is a relevant and tough case of intermittent runs of antidromic AVRT:
Wide Complex Tachycardia: is the patient stable or unstable?
===================================
MY Comment by KEN GRAUER, MD (4/24/2022):
===================================
Fascinating case sent in to us from Dr. Magnus Nossen, who is one of our frequent contributors. Dr. Nossen practices in Norway — therefore I always welcome his meticulously detailed cases that provide us opportunity to enhance our familiarity with the Cabrera Format, that is commonly used in Sweden (as well as regionally in parts of Norway, Finland, Japan, Italy — and in selected other areas of the world).
- For clarity — I’ve reproduced the initial ECG in today’s case — with the addition of the lead orientation used in the Cabrera Format in the bottom right corner of Figure-1 (For more on the Cabrera Format — See my ADDENDUM below).
- While I came to the same general conclusions about this case as did Drs. Nossen and Meyers — my perspective differed a bit regarding selected aspects of this case.
- Despite the near regularity in places — the reasons I immediately thought of WPW with very rapid AFib were i) As per per Drs. Meyers and Nossen — variation in QRS morphology is minimal, and far less than would be expected with PMVT (PolyMorphic VT); ii) Close scrutiny of the rhythm in the 6 chest leads (even without calipers!) — reveals a clearly irregularly irregular rhythm. (When I checked this rhythm more carefully in the comfort of my relaxing deskchair — calipers confirmed even more irregularly from one beat-to-the-next than was initially apparent); iii) Sinus P waves are absent — and most important — iv) The rate of the rhythm in Figure-1 is exceedingly fast — attaining 250/minute in many places (and occasionally attaining ~300/minute = as seen by the presence of R-R intervals as short as 1 large box in duration = 200 msec).
- Alternatively — Patients with WPW often develop the the AP-dependent reentry SVT rhythm known as AVRT (AtrioVentricular Reentrant Tachycardia). With accelerated anterograde conduction over the AP — AVRT may deteriorate to AFib (as was shown to occur in today's case during EP testing — and perhaps is also occurring in Figure-1?).
- The chest leads in V3, V4, V5 and V6 all show a distinct notching that I at first thought might represent atrial activity (Best seen in lead V4 — in which I've encircled 6 of these notches).
- That said — the fact that the rate of this notching was not regular told me that this was not AV dissociation (for which the atrial rate should be regular). Instead — these notched deflections are related (attached) to the QRS (Note constant distance between the peak of each notch [RED lines] — and the nadir of its neighboring QRS [BLUE lines]).
- Lead -aVR shows best that this notch appears to be part of the QRS (RED arrow in this lead).
- RED arrows in ECG #2 show return of sinus P waves, albeit with a short PR interval.
- As per Drs. Nossen and Meyers — there appear to be very subtle delta waves in a number of leads (BLUE arrows).
-USE%20copy.png) |
| Figure-2: I've labeled the initial ECG — and the 2nd ECG that was obtained after cardioversion (See text). |
- The 1st beat in this rhythm srip is conducted with a small-amplitude, upright in lead II P wave that looks different than the larger, upright P wave we saw in lead II of ECG #2 after conversion to sinus rhythm. So beat #1 in ECG #3 is probably not of sinus origin. The slender BLUE arrow nevertheless suggests there is preexcitation (a delta wave).
- There follows yet another P wave morphology which is pointed — and which appears to initiate a slightly irregular 12-beat run of ATach (Atrial Tachycardia) at ~140-150/minute. This run of ATach ends with the abrupt slowing of beat #14.
- QRS morphology of narrow beats #1, 2 and 14 is fairly similar to QRS morphology in the post-cardioversion tracing ( = ECG #2), in which there was no more than minimal preexcitation.
- As noted — I believe the BLUE arrow in lead II for beat #1 indicates a subtle delta wave. I don't see any delta wave or preexcitation for beat #2.
- QRS morphology begins to widen with beat #3 — and changes significantly beginning with beat #7. Comparison of QRS morphology of beats #7-thru-13 in each of the 7 leads shown in Figure-3 is very similar to QRS morphology in these same leads during the initial ECG (ECG #1), in which there was full preexcitation!
- Just as occurred for the 1st beat in this run of ATach ( = beat #2) — there is no preexcitation for the last beat in Figure-3 ( = beat #14), that also occurs after a brief pause.
- Various conditions affect the relative amount of preexcitation that may be seen at any point in time. This explains why despite the short PR interval in the post-cardioversion tracing (Figure-2) — delta waves are very subtle, and the QRS is not widened.
- This may also explain why even when you know a patient has WPW — you will not always see delta waves and QRS widening.
- Sinus rhythm is again present in ECG #4 (RED arrows in lead II). However, the PR interval is short — and delta waves are seen.
- Compared to ECG #2 — there is more preexcitation in ECG #4.
- And — compared to ECG #2 — the QRS complex in leads aVL and V1 in ECG #4 looks a bit more like the QRS morphology in these same leads during the full preexcitation tracing ECG #1.
-USE%20copy.png) |
| Figure-4: Comparison of QRS morphology depending on the relative amount of preexcitation (See text). |
- Despite AFib with a heart rate of over 200/minute in this 60+ year old woman — this patient remained hemodynamically stable with this arrhythmia! This highlights the important clinical point that some patients with WPW remain hemodynamically stable despite exceedingly rapid AFib rates for surprisingly long periods of time.
- The literature suggests that most patients with WPW who get into trouble as a result of AP-dependent tachyarrhythmias — do so by young adulthood (usually by 40 years of age). The clinical utility of this general rule — is that incidental discovery of WPW in an asymptomatic adult after middle age usually does not require intervention. Today's case provides us with an exception to this general rule — in that this previously healthy woman in her 60s presented with a potentially life-threatening arrhythmia (exceedingly rapid AFib) that required ablation of her Accessory Pathway.
- The usual amount of variation in QRS morphology and variation in heart rate that is typically seen in the ECG of a patient presenting with WPW-related AFib is not seen on the initial tracing in today's case. Instead — polymorphism and occasional obvious changes in heart rate are only seen later during the run of ATach that was caught on Telemetry monitoring (in Figure-3).
- EP testing in today's case induced AVRT, in which there was both antidromic and orthodromic conduction. The rhythm then degenerated in the EP lab to very rapid AFib. Regularity in the initial part of the tachyarrhythmia seen in Figure-1 — suggests a similar sequence of conduction changes may have occurred outside the EP lab in this patient — to which an additional supraventricular tachyarrhythmia (Atrial Tachycardia) was seen on Telemetry (Figure-3).
- Even when present — it is often difficult to identify delta waves during WPW-associated tachyarrhythmias.
The ECGs in Today's Case have been recorded using the Cabrera Format. It's easy to forget that electrocardiography is an international tool. While a standard ECG format (with no more than minor variation) is used throughout the United States — variations in format are used in a number of other countries.
- Several ECG parameters may vary in these other ECG formats. These most commonly include the speed of recording (ie, use of 50 mm/second — instead of the standard 25 mm/second speed used in the U.S.) — and — the sequence of the limb lead display (which is different in the Cabrera format — as is evident in the tracings shown above in today's case).
- Because we become accustomed to whatever ECG format is used in the country in which we practice — other ECG formats may be unfamiliar to us. As a result — the limb lead layout for the ECG shown in Figure-5 may have seemed strange when you first saw the initial ECG in today’s case. This is because the 1st limb lead displayed in Figure-5 is lead aVL — and, an aVR display occurs between leads I and II.
The Cabrera Format:
Initial description of the sequential limb lead format shown in Figure-5 was made by Fumagalli in 1949. Despite this — credit for this format is attributed to Cabrera. The Cabrera system has been in routine use in Sweden since 1977. A number of other countries also use the Cabrera format (ie, witness today’s case, contributed by Dr. Nossen from Norway). There are 2 Modifications in the Cabrera Format compared to the standard format used in the United States and in many (most) other countries: i) A recording speed of 50 mm/second is usually used in the Cabrera format; and, ii) A different limb lead sequence is used.
- As I “confessed” in the September 26, 2018 post of Dr. Smith’s ECG Blog — my brain is “programmed” to interpreting 12-lead ECGs and rhythm strips at the 25 mm/second speed that is standard in the United States. After 4+ decades of interpreting tens of thousands of tracings — there is an instant (automatic) process of "pattern recognition" that I find takes place in my brain, even before I begin systematic interpretation of any given tracing. This process is invalidated by the unfamiliar appearance of different-sized complexes that are produced when a 50 mm/second recording speed is used.
- NOTE #1: Other countries (such as Germany) often use a 50 mm/second recording speed. Usually it will be obvious on sight when a 50 mm/second speed has been used — but sometimes it won’t be. This is especially true when assessing narrow QRS rhythms for heart rate (ie, a narrow QRS rhythm may appear widened and excessively slow if you fail to recognize a 50 mm/second recording speed). Therefore — it’s important to be aware of the recording speed (and to clarify if the tracing you are interpreting is from a foreign country — especially if the recording speed isn’t marked at the bottom of the ECG).
- NOTE #2: Dr. Nossen was kind enough to convert the tracings that he submitted for today's case to the 25 mm/second speed that most of our readers are familiar with. Verification of recording speed was especially important in today's case — because accurate estimation of heart rate was the KEY clue for determining the rhythm in Figure-1.
-USE.png) |
| Figure-5: For the purpose of highlighting features of the Cabrera Format — I have reproduced the initial ECG in today's case, which I showed earlier as my Figure-1 (See text). |
The Altered Limb Lead Sequence in the Cabrera Format:
The insert in the lower right-hand portion of Figure-5 shows the rationale for the altered limb lead sequence in the Cabrera format.
- Rather than using lead aVR — the Cabrera format uses negative aVR ( = lead -aVR) — which is situated directly opposite (ie, 180 degrees away) from positive aVR. As shown in the insert of Figure-1 — lead -aVR is situated at +30 degrees (within the BLUE rectangle).
- In many ways — the Cabrera Format offers a much more logical display of limb lead sequencing. As opposed to the traditional U.S. format (in which limb leads are grouped into standard leads I,II,III — and augmented leads aVR,aVL,aVF) — there is gradually progressive (equally spaced) sequencing with the Cabrera format, beginning with the most superior lead viewpoint = lead aVL (at -30 degrees) — and moving gradually rightward (at 30 degree intervals) — until finally arriving at the most rightward placed lead = lead III (at +120 degrees).
- The Cabrera format enhances the clinical utility of aVR — by effectively adding lead –aVR as a transition lead between lateral and inferior frontal plane location. This allows greater specificity for determining the extent of high lateral and inferior lead ischemia or infarction. It also simplifies both axis and ST-T wave vector calculation in the frontal plane — since no more than a glance at the 6 sequential Cabrera leads is now needed for instant determination of which lead(s) manifests greatest net QRS and/or ST-T wave deflection. For example, in Figure-5 — Note how EASY it is to determine the frontal plane axis — because we can instantly see that the axis must lie between the two positive deflections (and closer to the largest positive deflection in aVL at -30 degrees, compared to the slightly smaller deflection in lead I at 0 degrees).
- Another potential advantage of the Cabrera format for limb lead sequencing — is that comparison with serial tracings in a given patient is easier. This is because the more gradually progressive Cabrera format for limb lead sequencing makes serial variation in Q wave presence, QRS amplitude, and ST-T wave displacements much more evident as to what represents probable “real change” — vs change in ECG waveforms that is more likely the result of some change in lead placement.
- BOTTOM Line: Despite the above potential advantages that may be derived from use of the more logical limb lead sequencing of the Cabrera format — it seems unlikely to replace the non-sequential traditional U.S. format, at least for the immediate future. Old established habits are difficult to break ... — even when a newer approach seems technically easy to implement and clinically advantageous.
================================
What IF the ECG is Recorded at 50 mm/second Speed?
IF you participate in international ECG forums — or otherwise have occasion to interact with colleagues who live in other countries — you will occasionally encounter ECGs recorded at the 50 mm/second speed. Because of the difficulty that I’m happy to acknowledge regarding the interpretation of arrhythmias and 12-lead ECGs recorded at 50 mm/second speed — I wanted to share a quick and easy way I’ve developed for “visually correcting” the wider appearance produced by a doubling of recording speed to 50 mm/second.
- The ECG in Figure-6 is taken from My Comment in the October 26, 2020 post in Dr. Smith's Blog. This multi-lead monitor recording uses Cabrera limb lead sequencing and a 50 mm/second recording speed (LEFT panel in Figure-6). Especially because of the shark-tooth ST distortion during the first half of the recording — I initially had trouble conceptualizing what I was seeing.
- PEARL: To compensate for the 50 mm/second recording speed — I uploaded this tracing to Power Point and: i) I reduced the width of this tracing by 50% (ie, from 10 inches to 5 inches); and, ii) I unchecked the "Keep Proportions" ( = "Lock aspect ratio" box) in the Format Pane under Size options in Power Point. Doing so narrows the width of the ECG by 50% without affecting the height. As can be seen in the RIGHT panel in Figure-6 — You’ll get twice as many little boxes (which must be considered when assessing rates and intervals) — but QRS complexes and ST-T waves now look "normal" to my eye.
 |
| Figure-6: This tracing (taken from the October 26, 2020 post in Dr. Smith's Blog) was recorded using the Cabrera format at a paper speed of 50 mm/second (LEFT panel). After “compensating” for 50 mm/second speed by reducing width of the tracing by 50% (without altering the tracing height) — the "visual appearance" of this ECG in the RIGHT panel now looks "normal" to my eye (See text). |

.jpg)


-USE%20copy.png)
No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.