This is from Amandeep ("Deep") Singh.
Dept Emergency Medicine, Highland Hospital, Oakland.
Case
51 yo male who walked to a
parked fire engine complaining of nausea and vomiting. Per patient, he started
feeling nauseous when he woke up, and shortly after, vomited.
On arrival at the emergency department, he reports that he has had intermittent episodes of chest pain associated with nausea and shortness of breath over the past 3 days. These episodes last about 20 minutes before spontaneous resolution.
He states that he is no longer having any chest pain, difficulty breathing, or nausea right now.
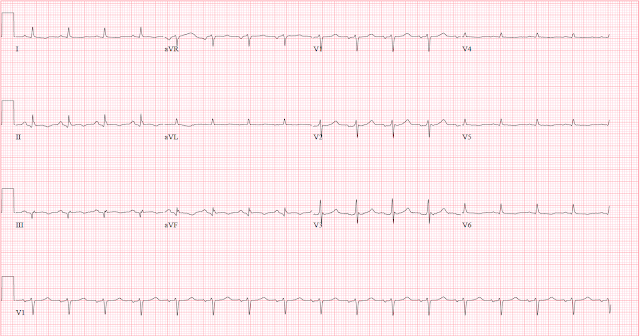
Here is his first ECG obtained in the ED.
The initial physicians interpreted with ECG as “no ST segment elevation” and ordered a cardiac work-up on the patient.
What do you think?
There are several subtle abnormalities on this ECG. The inferior leads show a Q wave, a fragmented QRS, subtle horizontal ST segment elevation (compared to PQ line), and T wave inversion. Lead I and aVL have a trace amount of ST depression and a slightly positive T wave. Lead V2 has a trace amount of ST depression and the hint of a prominent T wave. There is T wave inversion in V6. These findings are suggestive of a partially reperfused inferior-posterior MI and correlate with the resolution of his symptoms.
_________
Smith comment: this was sent to me with no information, and I responded: "Reperfusion of inferior and lateral MI, maybe also posterior." This is what I call "Inferior Wellens' syndrome." Wellens is a post-ischemic syndrome in which the chest pain is resolved and there are inverted (reperfusion) T-waves on the ECG; the significance is that while the patient had chest pain, the artery was occluded, but then spontaneously reperfused.
What stands out is the slight ST Elevation in II and aVF with convexity (called "coving") of the ST segment. The inversion of the T-wave suggests reperfusion. Any ECG showing reperfusion is VERY high risk, as that thrombus can propagate at any time and re-occlude.
___________
About 30 minutes after arrival, the patient reported chest pain, vomited, and appeared ill. His cardiac monitor was concerning for a wide-complex tachycardia and an ECG was obtained.
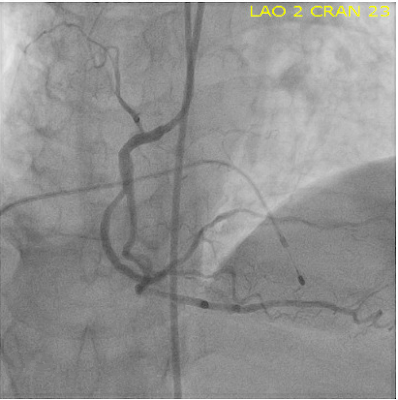
This rhythm was successfully cardioverted in the ED. His initial troponin returned at 2.46 ng/mL. He was taken to the cath lab where a 100% occlusion of the RCA posterior atrioventricular artery (TIMI flow 0) was identified and stented open. During the procedure he went into complete heart block and a brief episode of asystole lasting less than 1 minute.
A temporary transvenous pacemaker was placed.
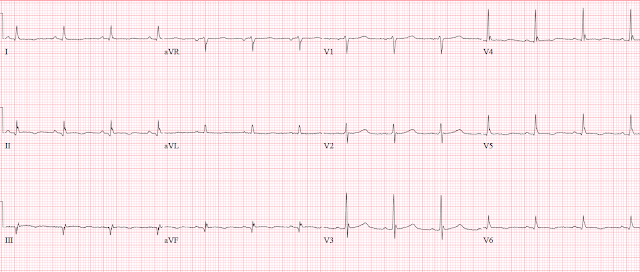
A review of the chart discovered this prehospital ECG which was not initially seen by the ED providers but was recorded by the fire department who initially evaluated the patient.
prehospital ECG found later:
Here there is more obvious ST elevation in lead III and a trace amount of ST elevation in aVF with reciprocal ST depression in leads I and aVL. There is also evidence of posterior extension of the MI with ST depression in V2-V4. There also appears to be trace ST elevation with T wave inversion in V6.
Here is the last ECG, after PCI the next day:
Learning Points:
1) we should learn how to identify ECG findings that can indicate partial reperfusion (e.g. findings in the case, Wellens T waves, AIVR)
2) Reperfusion is a prelude to re-occlusion
3) ED providers should try to locate the prehospital ECG on patients - they can help to expedite the appropriate care in some cases.
4) Learn to identify Subtle OMI
5) This very subtle OMI could have easily resulted in death (third degree heart block with asystole)
MY Comment by KEN GRAUER, MD (3/20/2022):
===================================
- The number of abnormal leads on the initial ECG.
- The low voltage on this tracing.
- Diagnostic points on the VT rhythm that followed.
Drs. Singh and Smith have detailed above why given the history of recent new chest pain — ECG #1 should have been recognized as diagnostic of recent infero-postero OMI, now showing reperfusion ST-T wave changes.
- I'll simply add the point we made numerous times on Dr. Smith's ECG Blog — namely that the more leads showing abnormal ST-T wave changes in a patient with new symptoms — the greater the concern for a recent or acute OMI (See My Comment and Table at the bottom of the page of the Sept. 13, 2020 post, among many others).
- No less than 11/12 leads in ECG #1 are abnormal. This includes the inferior leads (showing Q waves, ST coving with subtle elevation and developing T wave inversion) — lead aVL (showing a subtle mirror-image opposite ST-T wave picture as is seen in lead III) — lead V1 (with subtle ST flattening and a T wave that is taller than the T wave in lead V6!) — anterior leads V2,V3 (with subtle ST scooping suggestive of posterior involvement) — and lateral leads I, V4,V5,V6 (all of which show non-specific ST flattening with a hint of reperfusion T wave inversion).
The Low Voltage in ECG #1:
As I've emphasized in My Comment at the bottom of the page in the November 12, 2020 post of Dr. Smith's ECG Blog — true low voltage is not common. But it is present in both limb leads and chest leads in ECG #1.
- Among the potential causes of Low Voltage that I list in my Table from this Nov. 12, 2020 post — is myocardial stunning. Given sudden devopment of VT within 30 minutes of obtaining ECG #1 — I suspect myocardial "stunning" from the large acute OMI was the cause of this distinctly low voltage. In support of this hypothesis — is the finding of still reduced but larger QRS amplitudes in the ECG obtained on today's patient the following day after PCI (most noticeable in leads V3,V4 of that follow-up tracing).
As emphasized by Dr. Singh — the regular WCT ( = Wide-Complex Tachycardia) at ~230/minute seen in ECG #2 was clear indication for immediate synchronized cardioversion (that promptly restored sinus rhythm). Given the diagnostic challenge often posed by regular WCT rhythms — I thought it worthwhile to comment on why this tracing is virtually 100% diagnostic of VT.
- As we have often emphasized — Assume that any regular WCT rhythm without clear sign of sinus P waves is VT until you prove otherwise. IF you do so — you will be correct at least 80% of the time, even before you study ECG findings on the tracing. And if there is a clinical setting likely to predispose to VT (such as the acute OMI in today's patient) — then statistical likelihood of VT is >90% even before you look at the tracing!
- Added to this — the WCT rhythm in ECG #2 from today's case satisfies virtually all of my "quick recognition" criteria for VT (See My Comment in the May 5, 2020 post of Dr. Smith's ECG Blog).
- Is there “extreme” Axis deviation? By this I mean — Is the QRS complex during the WCT all negative in either lead I or in lead aVF? To emphasize that this criterion is of no benefit for distinguishing between VT vs SVT if there is any positivity at all for the QRS complex that you are looking at. Thus, in ECG #2 — there is a slight positive component to the QRS in lead I — therefore lead I by itself would not be of high enough specificity to confidently call this rhythm VT. But the QRS complex is clearly all negative in lead aVF! So, on the basis of lead aVF — this qualifies as "extreme" axis deviation — and before going further, already raises statistical likelihood of VT in today's tracing to >98%!
- Is there resemblance to any known form of conduction block? In ECG #2 — the QRS complex in lead V1 vaguely resembles RBBB morphology, in that the QRS is wide and upright — but the lack of any definition (ie, we see a formless monophasic R wave in lead V1) if anything, is more suggestive of VT than an SVT rhythm. Overall QRS morphology is "ugly" — by which I mean that QRS morphology in ECG #2 does not resemble any form of known conduction defect!
- Lead V6 is all negative. This is virtually never seen with a supraventricular rhythm (ie, it suggests that the electrical impulse begins in the apex).
- Lead aVR is all positive. This is also virtually never seen with a supraventricular rhythm (ie, it suggests that the electrical impulse begins in the apex).
- Is there relative “delay” in the initial QRS deflection? SVT rhythms tend to manifest more rapid initial depolarization vectors — because supraventricular depolarization generally begins its path toward the ventricles by travel over established conduction pathways. A notable exception to this generality is when there is an AP (accessory pathway) that bypasses the AV node (ie, in a patient with WPW). That said — the finding of “relative delay” in the initial portion of the QRS complex in multiple leads favors VT. Although sophisticated research studies cite a number of indices with precise initial deflection time limits as “accurate” criteria for VT — in practice, making precise millimeter measurements of initial QRS deflections at the bedside of a crashing patient is both time-consuming, and extremely difficult to accomplish with accuracy. In my experience — subjective measurements often suffice! That said, in ECG #2 — I found the biggest challenge was trying to precisely determine where the QRS complex begins. I believe there probably is at least some relative delay in the initial portion of most of the predominantly negative QRS complexes in ECG #2 — but this is clearly difficult to assess. (NOTE: Of the criteria I suggest in the above bullets — this last bullet regarding "relative delay" of the initial deflection is the most difficult to assess and in my experience, the least useful).
- BOTTOM Line: Except for my last criterion (regarding initial delay of widened QRS complexes) — each of the other criteria I state is positive for VT. I would therefore declare with 100% confidence that rhythm in ECG #2 was definitely VT.
- My attention was drawn to the inferior leads only by the morphology of the repolarization changes and NOT by any ST elevation. I would not put much store into ST deviations of that magnitude ( = less than 0.5 mm) — which, on considerable magnification on my computer — still remained very unconvincing.
- That said, the shape of the ST segments was very suggestive of a recent occlusion — and the T wave inversions (less than 0.3 mV) suggestive of partial reperfusion.
- I know Dr. Smith has mentioned an "inferior Wellens" before — but I had assumed that the T wave inversions would be of the same magnitude as those we see in the LAD occlusion of the original Wellens syndrome.
- The suggestion of ST depression in the right anterior precordials — though very, very subtle — was noticeable. I would not fault anyone less than a very experienced electrocardiographer for missing this one (based on these ECG changes). The history, however, provided more direction.
 |
| My Revised Wording — Regarding use of the concept of "extreme axis deviation" during a WCT rhythm for recognition of VT (Ken Grauer, MD). |




-USE.png)
No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.