This 40-something woman presented with severe anterior chest pain.
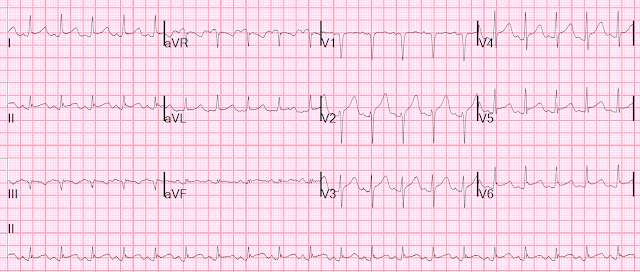
The prehospital ECG looked the same and the medics were worried about the ST Elevation and about STEMI/OMI.
What do you think?
There is ST Elevation that meets STEMI criteria in 3 consecutive leads V2-V4.
The T-waves in V2-V4 appear hyperacute.
The heart rate is 125!!
But, as we have discussed often, when there is tachycardia, you must doubt the diagnosis of acute OMI. Unless the OMI is resulting in decreased stroke volume, or there is an additional disorder, there should not be tachycardia. There must be another etiology or an additional processs.
What to do? Bedside Echo! POCUS.
Immediate POCUS showed a hyperdynamic heart with huge stroke volume.
Further evaluation revealed sepsis and the patient had bacteremia.
A formal echo was also normal.
Troponins were mildly elevated and this may be due to myocardial injury from sepsis or possibly to myocarditis. Follow-up ECGs were not done to prove presence or absence of evoltioin
See these cases:
Huge ST Elevation in V2 and V3. What is it?
===================================
MY Comment, by KEN GRAUER, MD (3/3/2022):
===================================
I was happy to see this case by Dr. Smith — because it reinforces in wonderful fashion a concept I've observed, but don't have good explanation for: Worrisome-looking ST elevation not due to acute coronary occlusion is sometimes seen with tachycardia.
- This worrisome-looking ST elevation often resolves when the heart rate slows.
My 1st impression on seeing today's tracing was obvious concern about the diffuse ST elevation. Features against an acute OMI included:
- Lack of any localization of this ST elevation (as is usually seen with acute infarction) — as the ST elevation in today's tracing is seen to some degree in all leads except aVR and V1.
- Lack of any reciprocal ST depression. ST elevation is maximal in lead V2 — so that IF this was acute LAD occlusion — it should be proximal enough to show some sign of inferior lead reciprocal ST depression.
- The marked tachycardia (as per Dr. Smith) — which IF this was true acute OMI from proximal LAD occlusion with a sinus tachycardia rate of 125/minute — I would have expected this patient to present in cardiogenic shock.
From another perspective — this ECG presents features consistent with acute Pericarditis (Please see My Comment at the bottom of the page in the December 13, 2019 post in Dr. Smith's ECG Blog). These include:
- Diffuse ST elevation.
- The ST-T wave appearance of lead II looks more like lead I than lead III.
- PR depression (best seen in leads I, II, V2,V3) — with PR elevation in aVR.
- No reciprocal ST depression
- An increased ST segment/T wave ratio in lead V6 (See My Comment in the Dec. 13, 2019 post).
MY Thoughts:
- True "pure" acute pericarditis is rare (A point often emphasized by Dr. Smith!). And this patient has septicemia!
- I suspect this patient may have a component of acute myocarditis in association with her septicemia.
- My academic curiosity would have loved to see follow-up tracings.
- BOTTOM Line: Worrisome-looking ST elevation not due to acute OMI may sometimes be seen in association with tachycardia. As per Dr. Smith — the presence of tachycardia in a patient not in cardiogenic shock shouldd make you rethink the diagnosis of acute OMI.

No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.