See Ken Grauer's important and detailed ECG analysis at the bottom.
Case
A 40-something with no PMH presented with palpitations, tachycardia, and crushing chest pain.
This was the prehospital ECG.
Idiopathic Ventricular Tachycardias for the EM Physician
Case Continued
No action was taken by the medics. She arrived in the ED and stated that she has had intermittent palpitations for almost one year. The episodes are generally associated with some mild dyspnea and one severe episode was associated with some substernal chest pressure type pain. They generally resolve in a matter of seconds to minutes. She has not sought any medical attention for this problem.
On the day of presentation, she had onset of palpitations approximately 3 hours prior and they were persistent since then. These episodes have lasted longer and felt more severe than any prior episodes. She had associated dyspnea and chest pain, described as a deep pressure like sensation. She also endorses some associated nausea and diaphoresis.
An ED ECG was recorded:
Toothache, incidental Wide Complex Tachycardia
Has been on an esmolol drip at a rate of as high as 50. Symptom and burden of nonsustained VT has been fairly controlled with esmolol drip and blood pressure has been stable. She did however continue to have significant arrhythmia burden increasing concern for approaching malignant form of RVOT VT. Cardiology following closely.
It is reassuring to see that there is no obvious structural abnormality that would suggest ARVD on at least echocardiogram. Management options discussed further conservative management/medical therapy versus invasive EP study and ablation procedure. Usually these arrhythmias do not respond well to beta-blockers and may end up requiring class Ic antiarrhythmic drug and pros and cons of that were also discussed.
She was later successfully ablated by the electrophysiologist. Troponins remained below the 99th percentile until after the ablation.
Idiopathic Ventricular Tachycardias for the EM Physician
REPETITIVE MONOMORPHIC VT (copied from UpToDate, an excellent resource for any physician)
REPETITIVE MONOMORPHIC VT — Repetitive monomorphic VT (RMVT) is characterized by frequent short "salvos" of monomorphic nonsustained VT (waveform 1). It was first described by Gallavardin in 1922 and is variously described in the literature as RMVT, RV tachycardia, RVOT tachycardia, catecholamine-sensitive VT, adenosine-sensitive VT, and exercise-induced VT. Approximately 10 to 15 percent of cases arise from the left ventricular outflow tract [26-28].
Although RMVT is considered to occur in "normal" hearts, static and cine-magnetic resonance imaging often reveal mild structural abnormalities of the RV, primarily involving the free wall (focal thinning, fatty infiltration, and wall motion abnormalities) [13-15]. The functional significance of these changes is uncertain. In the few cases studied, DNA from myocardial biopsies of ventricular muscle has been normal [29].
Epidemiology and clinical features — RMVT occurs almost exclusively in young to middle-aged patients without structural heart disease [1,2,4-9]. There has generally been no predilection on the basis of sex, although a 2:1 female predominance was observed in one report [26]. A surprising number of competitive athletes (particularly cyclists) are identified in many series of RMVT.
The most common associated symptoms are palpitations and lightheadedness during episodes [5,6]. In one illustrative report of 18 patients, twelve had symptomatic arrhythmia, two of whom had syncope, and six were completely asymptomatic.
Most arrhythmias are nonsustained (usually 3 to 15 beats), but up to one-half of patients have some sustained episodes, and some patients have only sustained VT [6,9,13,30]. (See 'Paroxysmal sustained VT' below.)
Bursts of nonsustained VT are typically provoked by emotional stress or exercise, often occurring during the "warm-down" period after exercise, a time when circulating catecholamines are at peak levels [5,6,8]. There may also be a circadian pattern, with prominent peaks between 7 and 11 AM and 4 and 8 PM, correlating with periods of increased sympathetic activity [31]. In some patients, a critical "window" of heart rates (upper and lower thresholds) that result in occurrence of the arrhythmia can be defined [27].
The inducibility of RMVT by stress or catecholamine infusion is suggestive of an abnormality in cardiac sympathetic function. Consistent with this hypothesis is evidence of regional cardiac sympathetic denervation in some patients with RMVT and structurally normal hearts (five of nine compared with zero of nine controls in one report) [32]. Patients with RMVT may also have regions of impaired neuronal reuptake of norepinephrine, leading to increased local synaptic catecholamine concentrations and downregulation of myocardial beta adrenergic receptors [33].
There may also be sex-specific triggers. In a report of 47 men and women with RMVT, states of hormonal flux (premenstrual, gestational, perimenopausal, administration of birth control pills) were the most common trigger for RMVT in 59 percent of women and were the only recognizable triggers in 41 percent [34]. Men were more likely than women to identify exercise, stress, or caffeine as a trigger (92 versus 41 percent).
Site of origin — RV tachycardias usually originate from the septal aspect of the RVOT [6,26,28,35-38]. A nine site mapping schema of the septal RVOT has proven useful in localizing RVOT tachycardias on the basis of their 12 lead ECG morphology (figure 1) [39].
RV tachycardias typically arise from a very narrow area just inferior to the pulmonary valve in the anterior aspect of the RVOT [37]. Endocardial mapping in such patients shows that the earliest site of endocardial activation occurs in this region [6,9].
Less commonly, sites of origin have been mapped to the RV inflow tract, the free wall of the RVOT, the root of the pulmonary artery, the left and right aortic sinus of Valsalva, the left ventricle, the mitral annulus, and the papillary muscles [26,36,38,40-49].
Electrocardiographic features — The typical rate of RMVT ranges from 140 to 180 beats/min, and may fluctuate based upon catecholamine levels. The VT cycle length often prolongs prior to termination.
RV outflow tract — The majority of RMVT episodes have a characteristic ECG appearance with two main features [1,2,4-9,39]:
●Left bundle branch block
●Inferior axis
This morphology is consistent with the RVOT origin seen by catheter ablation and endocardial mapping [6,37]. This ECG "signature" accounts for at least 70 percent of all idiopathic VTs [1].
The ECG pattern of RV tachycardia initiation may provide information about the site of origin and the arrhythmogenic mechanism as illustrated by the following observations:
●In a series of 32 patients with exercise-induced RMVT, VT usually began without a change in cycle length. Arrhythmias that initiated in this manner had an inferior axis, and appeared to be related to triggered activity due to delayed afterpotentials [50]. By comparison, VT initiated with a long-short sequence was more often nonsustained and often had a superior axis, suggesting an origin in the body or septal region of the ventricle; the mechanism for this VT is probably early afterpotentials.
●In a report of 14 patients, those with septal compared with free wall sites were significantly less likely to have notching of the QRS complex (29 versus 95 percent) and more likely to show early precordial transition by lead V4 (79 versus 5 percent) [51]. In addition, a positive R wave in lead I distinguished posterior from anterior septal and free wall sites.
●The degree of similarity of 12-lead ECG waveforms between VT and a pace map can be used to estimate the likelihood of successful ablation at that site. (See 'Radiofrequency ablation' below.)
Medical therapy — Medical therapy serves two roles in RMVT: termination of the arrhythmia; and prevention of recurrence. RMVT can be terminated with adenosine and beta blockers, all of which interfere with the cAMP-mediated slow inward calcium current [29,40,56-58].
For prevention of recurrence, beta blockers are often used as first-line agents. These drugs are attractive since their side effect profiles are mild in comparison with antiarrhythmic agents [64].
Propranolol has prevented recurrence in as many as 14 of 22 patients with a typical RVOT origin of RMVT [6,65]. However, other studies have found that these agents were much less likely to prevent recurrent RMVT, although the combination of a beta blocker with a class I drug may be useful [9,55].
Class I antiarrhythmic agents (table 2) alone are helpful in some patients. However, class III drugs (sotalol and amiodarone) may be preferred, especially in patients with arrhythmia that is refractory to other drugs [9].
Radiofrequency ablation — Due to the limited efficacy and potential side effects of antiarrhythmic drugs, there has been increasing use of radiofrequency (RF) ablation in patients with symptomatic RMVT. Professional society guidelines for the management of ventricular arrhythmias and the prevention of SCD indicate that there is evidence and/or general agreement supporting RF ablation in patients with symptomatic idiopathic VT that is drug-refractory, or in such patients who are intolerant of drugs or do not desire long-term drug therapy [64].
===================================
MY Comment, by KEN GRAUER, MD (2/14/2022):
===================================
Excellent case for illustrating the approach to a previously healthy "young-to-middle-aged" adult who presents in a sustained regular WCT ( = Wide-Complex Tachycardia) rhythm. For clarity — I've reproduced the initial tracing in today's case to highlight a number of additional points in the above presentation by Dr. Smith (Figure-1).
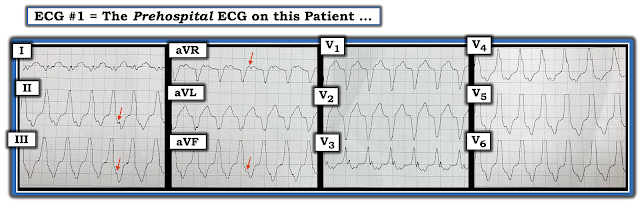 |
| Figure-1: — The initial ECG in today's case, obtained prior to arrival in the ED. |
The rhythm in Figure-1 — is a regular WCT at ~150/minute, without clear sign of sinus P waves The 1st question addressed — was to determine the etiology of this rhythm. Although impossible to be certain from this initial ECG alone — there are a number of clues that predict with high accuracy that the rhythm is RVOT VT (Right Ventricular Outflow Track Ventricular Tachycardia):
- There is a tendency to call regular WCT rhythms that resemble known conduction defects "aberrantly-conducted" SVT rhythms — especially when the patient is a younger adult without prior known history of heart disease. This is a mistake. The overall incidence of idiopathic VT (ie, VT in a patient who does not have underlying structural heart disease) — is ~10% in the general population. That said — this percentage increases in patients such as the otherwise healthy 46-year old woman in today's case — so that statistical likelihood that the regular WCT rhythm in Figure-1 is VT (even before assessing specific features of ECG morphology) — is probably ~20% (ie, high enough to actively consider VT in the differential diagnosis).
- NOTE #1: There may be retrograde atrial activity (ie, RED arrows in the inferior leads and in lead aVR possibly representing 1:1 VA conduction). That said — 1:1 retrograde conduction is not helpful in distinguishing between VT vs reentry SVT rhythms, because both may conduct with a 1:1 retrograde ratio.
- NOTE #2: For reference — I've summarized KEY points about the idiopathic VTs in Figure-2. Of the idiopathic VTs — RVOT VT is by far the most common form. ECG morphology of RVOT VT is described as resembling a LBBB pattern in the chest leads — and — an inferior axis in the limb leads (ie, much greater positivity of the QRS complex in inferior leads compared to lead I).
- Aberrant conduction most often manifests a QRS morphology consistent with block in one or more of the conduction fascicles, especially in patients without underlying heart disease. That is — QRS morphology with aberration in this previously healthy 46-year old should be expected to resemble a "typical" form of RBBB, LBBB, LAHB, LPHB or RBBB with one of the hemiblocks.
- QRS morphology in Figure-1 is not consistent with a "typical" LBBB pattern. Although predominant negativity in leads V1,V2 — and the monophasic R wave in leads V5,V6 are typical for LBBB conduction — the early transition (ie, all positive R wave already by lead V3) is not consistent with a "typical" preexisting LBBB pattern, because this conduction defect virtually always maintains predominant negativity at least until lead V5.
- Rate-Related LBBB Aberrancy in a previously healthy younger adult will also usually manifest a more "typical" LBBB morphology. In contrast — Left or Right Ventricular Outflow Track VT (ie, LVOT or RVOT VT) — will often manifest somewhat atypical LBBB morphology (often with earlier transition in the chest leads).
- The limb leads in Figure-1 are also not "typical" for the morphology of LBBB conduction likely to be seen with preexisting LBBB or aberrant conduction. Instead — there should be predominant positivity (usually a monophasic positive R wave) in leads I and aVL when there is an LBBB pattern from supraventricular conduction. The finding of a tiny QRS null vector in lead I, and an all negative QRS in lead aVL (as is seen in Figure-1) — strongly suggests that this rhythm is not supraventricular.
BOTTOM LINE: We should immediately suspect that the clinical presentation of this regular WCT rhythm without sinus P waves, in this previously healthy 46-year old woman — with "atypical" features for LBBB conduction — is not representative of SVT with LBBB aberration. Instead — the clinical presentation and ECG morphology seen in Figure-1 is completely typical for the presentation of RVOT VT until you can prove otherwise.
-USE%20copy.png) |
| Figure-2: Review of KEY features regarding Idiopathic VT (CLICK HERE — for the source of this Summary). |
For MORE on Idiopathic VT:
- CLICK HERE — to listen to my 8-minute Audio on Pearls for ECG Recognition of Idiopathic VT (with special attention to RVOT VT and Fascicular VT — which are the 2 most common forms).



No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.