Written by Pendell Meyers
A man in his early 60s presented with acute chest pain rated 10/10 with associated nausea and vomiting with known history of multivessel CAD. He presented at 2300 with onset of symptoms at 2230. He was awoken from sleep by the symptoms, which were identical to prior MI for which he received a stent years ago. On arrival his heart rate was 43 bpm and blood pressure 91/62. Atropine and IV fluid was given.
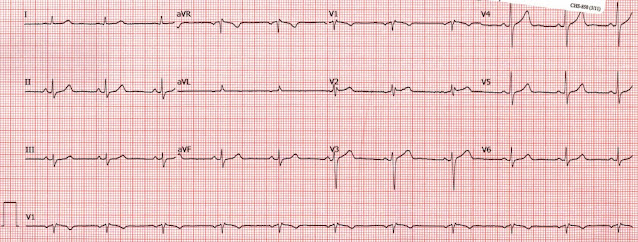
Here was his triage ECG:
 |
| What do you think? Baseline below for comparison, but try first without it. |
His baseline ECG was available on file:
The presentation ECG shows diagnostic evidence of posterolateral OMI. There is sinus bradycardia with a relatively normal QRS complex, followed by some STE in aVL, with upright hyperacute T wave, with reciprocal STD in the inferior leads and negative hyperacute T waves. The posterior involvement is suggested by STD in V3-V4, which is highly specific for posterior OMI in the setting of ACS and no QRS explanation (RVH, RBBB, etc.) for such STD.
This ECG is very easy for readers of this blog. But it does not meet STEMI criteria.
The EM providers evaluated the patient and concluded, easily, that the patient was having ACS. But they did not understand the ECG, documenting "no clear STEMI."
CT pulmonary angiogram was chest negative for PE.
Initial troponin I was 15 ng/L (99% upper reference limit for men is 20 ng/L for this assay). Remember how his symptoms started just 30 minutes prior to arrival!
Repeat troponin I was 21 ng/L (delta = 6 ng/L, dangerously close to our departmental delta value of 4 ng/L!)
Another ECG was obtained at 2330:
 |
| Ongoing posterolateral OMI. |
ASA and heparin were started, as well as nitroglycerin drip, none of which controlled his ongoing chest pain. He was then given 4 mg morphine x 2.
The EM physician then initiated code STEMI due to "continued minimal ST elevation in aVL and ongoing pain and vomiting." An emergent transfer is initiated to the nearby cath center. Cardiology "canceled" the code STEMI, but accepted the patient for urgent transfer.
Cardiology documents:
"ECG was not definitive for STEMI but there was concern for an acute circumflex lesion given the lack of definitive ECG changes but typical presentation."
"NSTEMI with unstable angina. EKG with NSR with ST depression in III and aVF. Chest pain starting at 2230 and remaining constant despite nitrates, heparin, aspirin, and morphine."
Angiogram at 0230 (4 hours after arrival):
LCX proximal 99% stenosis with thrombus, TIMI 3 flow, at the edge of a previously placed stent. The lesion was stented with excellent angiographic result. EF at cath was 55%.
"To be clear this was not a STEMI presentation given the lack of ST elevations and TIMI-3 flow on angiography but an emergency procedure was indicated as the patient had intractable chest pain with non-STEMI with intractable unstable angina. Patient does not need to go to an ICU."
Meyers comment: There are several problems with this cardiologist's last comment that reveal significant gaps in understanding of AMI and ACS. The cardiologist states very clearly that he or she believes TIMI-3 flow is not possible with "STEMI." This is obviously false, here is an excerpt from our recent study:
Outcomes used to ascertain the presence of OMI on the ECG cannot be based solely on TIMI flow of the lesion at the time of the angiogram because the state of the artery frequently differs between the time of the ECG and the time of the angiogram. Proven STEMI has an open artery in 19% to 36% of cases, depending on whether it is TIMI −1, −2, or −3 flow. Karwowski et al showed that only 64% of 4581 STEMIs had TIMI 0 flow on angiogram. [25] Stone et al found that 72% have TIMI 0 or 1 flow. [26] Finally, Cox et al found that 80% had TIMI 0, 1, or 2 flow.[26] Thus, approximately 20% of true, obvious STEMIs have TIMI 3 flow at immediate angiogram. [27]
25. Karwowski J, Gierlotka M, Gasior M, Polonski L, Ciszewski J, Beckowski M, Kowalik I, Szwed H. Relationship between an in-farct related artery, acute total coronary occlusion, and mortality in patients with ST-segment and non-ST-segment myocardial infarction. Pol Arch Intern Med. 2017;127:401–411.
26. Stone GW, Cox D, Garcia E, Brodie BR, Morice MC, Griffin J, Mattos L, Lansky AJ, O’Neill WW, Grines CL. Normal flow (TIMI-3) before mechanical reperfusion therapy is an independent determinant of survival in acute myocardial infarction: analysis from the primary angioplasty in myocardial infarction trials. Circulation. 2001;104:636–641. doi: 10.1161/ hc3101.093701
27. Cox DA, Stone GW, Grines CL, Stuckey T, Zimetbaum PJ, Tcheng JE, Turco M, Garcia E, Guagliumi G, Iwaoka RS, et al. Comparative early and late outcomes after primary percutaneous coronary intervention in ST-segment elevation and non–ST-segment elevation acute myocardial infarction (from the CADILLAC Trial). Am J Cardiol. 2006;98:331–337. doi: 10.1016/j.amjcard.2006.01.102
Case Continued:
Echo next morning:
EF 50%. Akinesis of the basal-mid anterolateral, inferolateral, and inferior myocardium.
Repeat troponin I in AM: greater than 25,000 ng/L (our lab's upper reporting limit)
The patient had an uncomplicated hospital course and was discharged.
Learning Points:
Expert ECG diagnosis could have dramatically improved the patient's time to reperfusion.
LCX OMIs are the most frequently missed. NSTEMI patient with missed OMI have double the mortality compared to NSTEMI patients without OMI. This patient was not completely "missed", but significantly delayed (approximately 3.5 hours) due to lack of expert ECG interpretation, and potentially sluggish recognition of refractory angina and ECG ischemia, and cancellation of emergent transport.
This patient provides an example of OMI with an initial high sensitivity troponin I less than the 99%ile upper reference limit, as happens in 1/4 of all true STEMI (Wereski et al.--Smith is a co-author).
ACS with ongoing pain and/or ECG ischemia despite medical management has always been an indication for emergent (less than 2 hours) cath, in all guidelines; however, this guidelines is not frequently followed.
I will repeat this important point: "STEMI" does not require TIMI 0 flow. About 20% of obvious STEMI(+) OMI patients have TIMI 3 flow at the time of angiogram. TIMI 3 flow at the time of cath cannot be used as a reason why a patient didn't have OMI or STEMI.

No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.