Written by Pendell Meyers
A woman in her 60s was shopping when she suddenly experienced palpitations and chest "discomfort." She denied outright chest pain or dyspnea. She walked across to the street to my Emergency Department. She had no known prior history of dysrhythmias or heart disease, but had known hypertension, breast cancer, diabetes, and obesity. She has had episodes of palpitations in the past, followed by holter monitor workups which did not reveal any cause of palpitations. However, her symptoms today feel worse than prior episodes, and she has never felt the "chest discomfort" with prior palpitations. Upon pointed questioning, she told the providers she has had several similar episodes over the past few weeks, but did not seek care during those episodes and they were shorter.
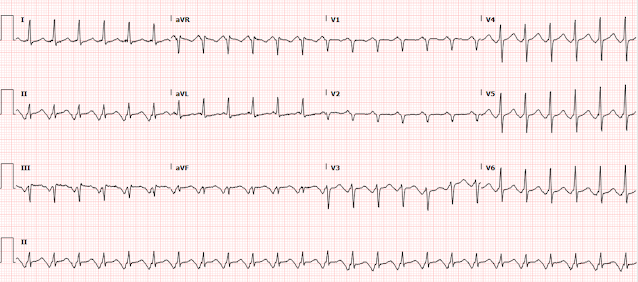
Here is her triage ECG during active persistent symptoms:
 |
| What do you think? |
Two high sensitivity troponin I measurements were less than 6 ng/L.
The cardiology team incorrectly diagnosed this rhythm as atrial flutter with 2:1 block.
She was admitted for rate control and "new onset atrial flutter workup."
Echo was normal.
Unfortunately, in the mindset of atrial flutter, the patients CHADS2VASc score was calculated at 3, and she was deemed to require anticoagulation with eliquis (apixaban), which she has been on ever since (several months at this point). I am trying to contact her providers to discuss this.
She was also placed on metoprolol, presumably for rate control during her perceived atrial flutter episodes. In reality, it may be suppressing her SVT (whether it is ectopic atrial tachycardia or AVNRT).
Check out these posts showing atrial repolarization (Ta wave) and how it can cause inferior pseudoSTEMI/OMI patterns:
A man in his sixties with chest pain
Look at this ST Depression (It's not real)
Atrial Repolarization wave mimicking ST Elevation:
Sudden CP and SOB with Inferior ST Elevation and in STE in V1. Is it inferior and RV OMI?
A man in his sixties with chest pain
Learning Points:
Atrial repolarization can be especially visible in ectopic atrial tachycardias (or any dysrhythmia with pronounced ectopic atrial waves), causing the appearance of inferior STE that has nothing to do with OMI.
Diltiazem should not generally cause conversion of atrial flutter to sinus rhythm. Diltiazem converting the rhythm would be more consistent with a reentrant dysrhythmia involving the AV node, such as AVNRT. There is always a chance that the conversion was actually just spontaneous and not associated with the diltiazem.
Misdiagnosis of atrial flutter can lead to significant long term patient harm, especially when treated with anticoagulation. Sometimes getting the rhythm correct is very important.




No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.