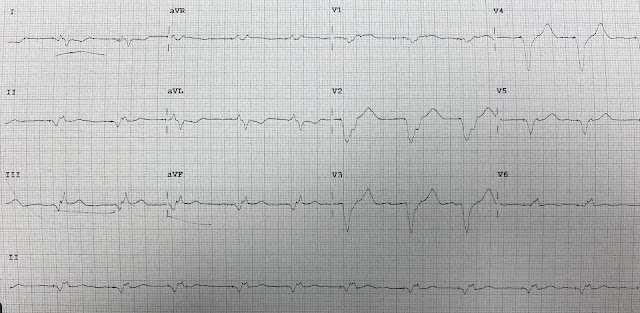
I was texted this ECG with the info that the patient "clinically looked like he was having a myocardial infarction":
There is atrial and ventricular pacing. Both spikes are best seen in V1 and V2 (as always, if you click on the image, it enlarges). The QRS is very very wide. On the image below, I have drawn lines in every lead from the QRS onset (blue) and QRS end (red). I measure the QRS duration at about 280 ms. Of course, all ventricular paced rhythm is wide, but not often this wide. One must always consider hyperkalemia when the QRS is very wide, but the K turned out to not be high.
Here is the EKG with blue lines at the QRS onset and red lines at QRS end:
Beside the pacing and wide QRS, there is no significant concordant ST Elevation, and no excessively discordant ST elevation or depression (in other words, it does not meet the Smith Modified Sgarbossa criteria, even at the 20% ratio).
There is possible trace STE in III and reciprocal STD in aVL.
There is Pseudo ST Depression in V2, but as you can see from my lines, that is QRS, not ST segment.
There is also QRS fragmentation (see especially leads II, III, aVF). This is a good sign of ischemic heart disease, and analogous to Q-waves of MI. In combination with the very long QRS, my reply to the text message was this:
There is QRS fragmentation, but no evidence of acute OMI or acute ischemia. The wide QRS and fragmentation suggest that this patient has ischemic cardiomyopathy. Of course, ischemia, and even OMI, may not manifest on the ECG, whether in the context of paced rhythm or normal conduction. The patient may have chronically elevated troponins with this cardiomyopathy.
More history was obtained:
A male in his 60s with h/o dialysis, peripheral arterial disease, coronary disease, and sick sinus syndrome with pacemaker complained of onset of chest pain and vomiting. His systolic blood pressure was in the 80s and he "looked like he was having a heart attack." After a complete workup, including a bedside POCUS which showed poor ejection fraction, the clinicians were convinced that the patient was having a myocardial infarction, and that was reinforced by their interpretation of the ECG as "showing an inferior MI."
Smith opinion: There is no ECG evidence of acute ischemia. However, unless another etiology of chest pain and hypotension can be immediately found, one must assume that this is high risk ACS in spite of the absence of ACUTE findings on the ECG. The patient should be taken for angiogram. The ECG clearly shows the presence of coronary disease.
They activated the cath lab thinking there was an inferior MI (Smith aside: I do not think this ECG shows inferior MI).
The cath team decided not to take the patient. They did not come up with an alternative explanation for the chest pain and hypotension.
Smith comment: I can understand that if a patient presents with chest pain and has no objective evidence of ischemia (EKG or troponin rising/falling), then one might blame it on esophageal reflux. But hypotension and shock need an explanation. If you have acute chest pain, ECG and echo evidence of ischemic cardiomyopathy, low ejection fraction, and no other explanation, then you must rule out a coronary etiology with an angiogram.
Troponins, with discussion:
His troponins later returned: Initial troponin T was 0.088 ng/mL and 2.5 hours later it was 0.091 ng/mL.
It would not be surprising if this patient had chronically elevated troponins, and indeed at a different hospital on a previous visit, the patient had these serial troponins measured (contemporary, 4th generation, troponin I -- manufacturer unknown):
Previous visit, Troponin I: 0.124 ng/mL ➡️ 0.127 ng/mL ➡️ 0.129.
These previous steady state Troponin I further support chronically elevated troponins. Nevertheless, because troponin I and T are very different and no two assays can be directly compared, we cannot determine whether the troponins on this visit (the present one) are, or are not, more elevated and thus could represent acute on chronic elevation. There is no rise and/or fall, which usually (but not always) indicates that they are chronic (called "chronic myocardial injury," and common in cardiomyopathy). Sometimes there is an acute rise and the 2 values are measured on either side of a peak and so do not show rise and/or fall. Furthermore, troponin I and T do NOT correlate well with each other. Trop I is often a 5-10x larger number than trop T. Therefore, trop T of 0.088 ng/mL and 0.091 ng/mL might indeed be high compared to the previous visit (which was trop I), but this is uncertain.
Thus, if this is ACS, it is possible that it is acute MI, but if not, it could very well be unstable angina, which still exists even in the era of high sensitivity troponin. See Thelin reference below, with comment, and this blog post: "Unstable Angina still exists", even in the Age of High Sensitivity Troponin
Outcome:
Four hours later, the patient had a ventricular fibrillation arrest and the patient could not be resuscitated.
In acute coronary syndrome, the ECG frequently does not manifest ischemia. If the patient looked like he was having an MI, and there is no other explanation, especially if he is hypotensive with poor myocardial contractility, then you treat it as such and take the patient to the cath lab. That is why the ACC/AHA guidelines state that emergent cath lab activation may be necessary in an unstable patient even in the absence of STEMI, and the European guidelines say that many patients need < 2 hour angiogram “even in the absence of EKG or biomarker evidence of infarction.”
Here is a quote from the guidelines at this link:
See page 2367
4.4. Ischemia-Guided Strategy Versus Early Invasive Strategies
See Figure 3 for the management algorithm for ischemia guided versus early invasive strategy.
4.4.1. Early Invasive and Ischemia-Guided Strategies
For definitions of invasive and ischemia-guided strategies, see Table 8.
1. An urgent/immediate invasive strategy (diagnostic angiography with intent to perform revascularization if appropriate based on coronary anatomy) is indicated in patients (men and women¶) with NSTE-ACS who have refractory angina or hemodynamic or electrical instability (without serious comorbidities or contraindications to such procedures).40,42,173,174 (Level of Evidence: A)
2. An early invasive strategy (diagnostic angiography with intent to perform revascularization if appropriate based on coronary anatomy) is indicated in initially stabilized patients with NSTE-ACS (without serious comorbidities or contraindications to such procedures) who have an elevated risk for clinical events (Table 8).40,42,173–177 (Level of Evidence: B)
Summary:
“Refractory angina should go to the cath lab within 2 hours”
Also:
Hemodynamic instability
Electrical instability
Worsening Heart Failure
High Sensitivity Troponins and Unstable Angina
There was no rise and/or fall of troponin in this case, so it does not meet the definition of myocardial infarction. These troponins were NOT high sensitivity (hs) troponin, but that does not matter. However, even in the era of hs troponin, unstable angina still exists. Here I describe one study which used the Roche hs-cTnT assay.
Thelin et. al. Eur Ht J, Acute Card Care 2014; 4(5):403-9
• Initial hs-cTnT among 478 patients presenting with chest pain as the primary symptom
• 160 (33.5%) had initial value below 5 ng/L
• NPV of 100% for NSTEMI (70 NSTEMI; 37 UA)
• NPV of only 94% for any ACS (includes Unstable Angina)
• Sensitivity 91% (80-95)
– Missed 10 of 107 ACS as diagnosed by angiography; 8 PCI
• Clinical judgment and pre-test probability of ACS is critical


What a sad and unfortunate case.
ReplyDeleteTwo questions if you dont mind!
1) about the modified Sgarbossa criteria. Did you study the specificity for concordant ST-depression in any lead (other than v1-v3) for OMI? One could think there's a hint of ST-depression in lead aVL and, if it were real, it would be concordant depression. But is concordant depression any good for recognizing OMI, any idea?
2) The AHA guidelines state: Urgent/immediate invasive strategy is indicated in patients who have "refractory angina". What does this refractory angina actually mean? Recurrent/persistent chest pain/symptoms of ACS? Does it include recurrent/persistent ischemic ST-depression? Every now and then I think we all see patients who (after receiving aspirin, ticagrerol, nitro-drip etc...) state that the pain is gone or just a little soreness, but the ECG show ischemic ST-depression (NSTEMI equivalent with no evidence of OMI), a little less depression than before but nevertheless at least some ischemic ST-depression. Does this mean the patient has "refractory angina" and the cathlab should be activated by the guidelines? thanks!
1. See reply below.
Delete2. Refractory angina means that if you think the patient is having myocardial ischemia in spite of absence of objective evidence (EKG or troponin), then you should still activate the cath lab and look at the coronaries.
In a centre without cath lab, would thrombolysis be the alternative option of management?
ReplyDeleteIn a centre without cath lab, would thrombolysis be the alternative treatment option?
ReplyDeleteYes, I would give tPA.
DeleteDr. Smith, thanks for yet another challenging case ( jAN 17th 2021 Sunday ). Going by the BARCELONA
ReplyDeletecriteria to diagnose MI in LBBB, and going by the commonly agreed policy of extrapolating to RV
paced rhythm like in our case, we are getting 1) concordant ST depression of 1mm in Lead I AND
2) CONCORDANT ST depression of 1mm in Lead aVL - SUFFICIENT TO CONCLUDE that there is MI. Also kinly note that when Lead aVL is vertically flipped. the QRST complex looks stunningly similar to Lead III. With regards, Dr.R.Balasubramanian. Pondicherry - INDIA
I disagree that there is 1 mm STE. That said, < 1 mm STE is fairly specific for OMI in LBBB, though not as specific as 1 mm. But the point is that you do not need to meet any LBBB/VPR OMI criteria in a case like this. The clinical situation is plenty to activate the cath lab and do an angiogram. Insisting on meeting EKG criteria that are not there does not help future patients with similar clinical presentations, in which the interventionalist will (accurately) reply that it does not meet "criteria".
Deleteinteresting case, steve. point taken: if he patient is showing persistent ischemia/chest pain/ and is hemodynamically unstable , needs cath.
ReplyDeletein our shop that's TNK (tenectaplase) and ship to PCI center.
question: i thought a few years ago, we thought that in cardiogenic shock, lytics were not indicated. is that incorrect?
thanks for another excellent teaching case.