A 40-something man with Hx of treated HTN had chest "squeezing," with SOB and diaphoresis, 10 hours prior to presentation. It lasted 5 minutes then resolved. There was an exertional component. Then, 1 hour before arrival, it recurred, again lasting 5 minutes. His 3rd and last episode was worse, had radiation to both arms, and was 10/10.
911 was called and this prehospital ECG was recorded at time zero:
Limb leads:
911 was called and this prehospital ECG was recorded at time zero:
Limb leads:
 |
| Note the artifact that is simultaneously recorded in all limb leads. This was mistaken by the treating physicians for ST depression initially. |
 |
| What do you think? |
This is diagnostic of LAD OMI. There is STE that does not meet STEMI criteria in V1-V6. There are normal size T-waves in V1-V3, but these T-waves are enormous relative to the QRS amplitude. These are hyperacute T-waves. Moreover, any time there is ST Elevation of any amount, it must be explained: is it normal STE? Or ischemic?
One sign that eliminates the possibility of normal STE is "Terminal QRS distortion." That is the absence of both an S-wave and a J-wave in EITHER V2 or V3. Here there is no S-wave in V3 and also no J-wave. This is diagnostic of ischemic STE and of LAD OMI.
See these previous posts on Terminal QRS distortion:
Paper published: Terminal QRS distortion not found in any ECG of Early Repolarization
Best Explanation of Terminal QRS Distortion in Diagnosis of Electrocardiographically Subtle LAD Occlusion
4 Cases Discussing Terminal QRS Distortion in Diagnosis of Anterior MI
Case continued:
The patient received a sublingual NTG and his pain resolved (is this a result of NTG? Or coincidental? -- unknown).
This pain free ECG was recorded:
 |
| All STE is resolved. The S-wave in V3 is restored! The artery has reperfused If you didn't believe it before, then this dynamic ECG proves it. |
He had multiple subsequent prehospital ECGs, all identical to the last one and all pain free.
He received an aspirin.
On arrival, this was recorded:
 |
| Normal |
Cardiology was consulted and they did not want to take the patient to the cath lab emergently.
Heparin was given.
A POCUS cardiac showed no WMA.
First troponin was 0.042 ng/mL (elevated above 99th %-ile URL of 0.030 ng/mL).
1.5 hours later, this ECG was recorded:Heparin was given.
A POCUS cardiac showed no WMA.
First troponin was 0.042 ng/mL (elevated above 99th %-ile URL of 0.030 ng/mL).
 |
| Still normal |
Several more were recorded, with no change.
This was recorded at 8 hours:
This was recorded the next AM:
 |
| Evolution of Wellens', with more widespread and deeper T-wave inversion. |
See this:
Classic Evolution of Wellens' T-waves over 26 hours
And a bit of further evolution here.
Troponin profile
The patient underwent angiography and had a 90% thrombotic proximal LAD lesion that was stented.
Here is his formal echo report:
Normal left ventricular size, mildly increased concentric left ventricular wall thickness and normal systolic function.
The estimated left ventricular ejection fraction is 61 %.
There is no left ventricular wall motion abnormality (WMA) identified.
This patient's ischemia was so brief that it did not cause any myocardial stunning. It is common to have a persistent WMA after resolution of ischemia (thus, the ECG is a better indicator of instantaneous ischemia than echo), but we see here that a normal echo does not rule out transient STEMI/OMI.
This patient's ischemia was so brief that it did not cause any myocardial stunning. It is common to have a persistent WMA after resolution of ischemia (thus, the ECG is a better indicator of instantaneous ischemia than echo), but we see here that a normal echo does not rule out transient STEMI/OMI.
===================================
Comment by KEN GRAUER, MD (9/22/2019):
===================================
There are important concepts to emphasize in this case by Dr. Smith. I focus my attention on the first 2 ECGs, both of which were done prior to arrival in the hospital.
- For clarity — I’ve put the 2 pieces of the 1st ECG together, and I’ve relabeled the tracings (Figure-1).
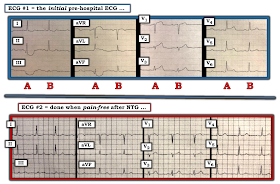 |
| Figure-1: The first 2 ECGs in this case (See text). |
The 2 ECGs in Figure-1 were obtained prior to arrival in the ED. The patient is a 40-something year old man with new chest pain.
- ECG #1 shows a regular sinus rhythm with narrow QRS complexes. The QTc is normal. There is no chamber enlargement. R wave progression is normal. The most remarkable findings (as per Dr. Smith above) — are the ST-T wave changes.
QUESTION: WHY is there so much difference in the appearance of QRS complexes and ST-T waves occurring every-other-beat in ECG #1? That is, WHY does the 1st QRST complex in each group of 3 leads (beats labeled “A”…) — look so different compared to the 2nd QRST complex (beats labeled “B” in ECG #1)?
MY ANSWER: I believe every-other-beat in ECG #1 is altered by Artifact! While it clearly is more difficult to recognize this in the chest leads — it should be obvious from the limb leads that the beats labeled “A” are greatly influenced by Artifact.
- Although beat A in lead I is not affected — the bizarre, scooped depressions of the entire ST segment for beat A in leads II and III of ECG #1 are clearly artifactual. This tells us that the Q wave seen in lead II for beat A (but not for beat B) is not real.
- Similarly — it should be obvious that the Q wave and bizarre, scooped depression of the entire ST segment for the beat labeled “A” in lead aVF is largely altered by artifact. The extra scooped ST elevation for “A” in lead aVR is also largely altered by artifact. A little less obvious, but still quite evident is the artifactual ST elevation for “A” in lead aVL.
- In the CHEST LEADS — IF you look closely — the T waves for beats labeled “A” in leads V1, V2 and V3 are all taller (more prominent) than the T waves for beats labeled “B” in these leads. The reasons I believe beats A in V1, V2 and V3 are altered by artifact are: i) that the shape of the ST segments for beats labeled A in leads V1 and V2 looks unnatural (ie, it looks to me to be artifactually distorted); and, ii) the every-other-beat cadence of artifact is CONSISTENT throughout ECG #1 for each of the beats labeled “A” — whereas beats B throughout ECG #1 do not have the appearance of artifact.
- Even more subtle, is the alteration by artifact of beats labeled “A” in leads V4, V5 and V6. Note that there is slight-but-real ST elevation and increased prominence of the T wave in each of these lateral chest leads for beats labeled “A” compared to those labeled “B”.
PEARL #1: It’s important to suspect artifact whenever you see unusual (unexpected) alterations in QRST morphology — because this may significantly affect your interpretation!
- IF, as I suspect — every-other-beat in ECG #1 is indeed altered by artifact — then both the ST elevation seen in each of the chest leads for beats labeled “A” — and, the terminal QRS distortion for beat A in lead V3 may not be real (ie, Note that the S wave does descend below the baseline for beat “B” in lead V3 — as it normally should do when there is an S wave in this lead).
- I admit that I am not certain why altered QRST morphology is occurring at a cadence of every-other-beat for the 8 beats we see in ECG #1 (possible intermittent tremor in the left foot — judging by maximal artifact in leads II, III and aVF). That said — IF you recognize this inconsistency in QRST morphology that is occurring every-other-beat — it could be EASY to find out if I am correct in suspecting artifact by: i) Immediately repeating the ECG, to see if this every-other-beat occurrence goes away! — and, ii) Looking at the patient while you repeat the ECG (sometimes you’ll see patient movements or other occurrences at the bedside that immediately make obvious the cause of artifact).
PEARL #2: Regardless of whether I am correct or not that beats labeled “A” in ECG #1 are altered by artifact — the T waves labeled “B” in leads V2 and V3 are disproportionately tall and fatter-than-they-should-be-at-their-peak given the diminutive amplitude of the QRS complex in these 2 leads. In addition, the upright T wave for beat “B” in lead V1 is more prominent than it should be — especially since T wave amplitude of B in V1 is greater than T wave amplitude of B in lead V6! (Normally T wave amplitude in V6 should be greater than in lead V1.). In a patient with new chest pain — these T wave changes for beats labeled “B” in leads V1, V2 and V3 constitute hyperacute T waves!
- Note in ECG #2 done a little while later (after sublingual NTG relieved chest pain) — that there is no longer variation in QRST morphology occurring every-other-beat. This supports my suspicion that beats labeled "A" in ECG #1 were altered by artifact.
- Comparing QRST morphology seen in ECG #2 — with QRST morphology in each of the 12 leads for beats labeled “B” in ECG #1 (which I believe were the beats without artifact) — shows subtle-but-real improvement in the hyperacute anterior lead T wave appearance we saw for beats “B” in ECG #1. That said — there is decidedly less change between these 2 ECGs than might be thought if one simply compared ECG #2 with beats labeled “A” in ECG #1.
I wish ECG #1 would have been repeated immediately — while looking at the patient to see if a cause for the artifact I suspect might have been identified.
Our THANKS again to Dr. Smith for this instructive case!




To me, it appears that there is also (strange) artifact in the precordial leads of the EMS ECG as well as the limb leads. The 2nd complex in each of those leads appears very similar to the follow up ECG's (ex. V3 has an S-wave). If not artifact, what else would cause the large beat-beat variation?
ReplyDelete@ Unknown — I suspect you sent your excellent question in BEFORE I wrote My Comment. As I illustrate above — I believe ALL of the beats labeled "A" in ECG #1 (in my Figure-1) are influenced by artifact. Please read My Comment — and write us back if you still have any questions! — :)
DeleteAgree, there is some artifact.
DeleteNice case! I agree with Dr Grauer that even the first complexes in the chest leads likely are affected by artifact. My guess would be that something is happening with the left leg electrode, since lead I is the only lead which is identical between A and B. The artifact affects WCT and thus the changes seen in the chest leads in A are likely also artifactual, including the finding of TQRSD.
ReplyDeleteIt is interesting that no T wave inversion is present after NTG when the patient is pain free, considering Wellens syndrome, which is beautifully shown in the later ECGs.
/Thomas
@ Thomas Lindow — THANK YOU for your excellent comments! I expand upon determining which lead is most likely the source of artifact in the very next Blog post (from Sept. 27 — https://hqmeded-ecg.blogspot.com/2019/09/chest-pain-with-nondiagnostic-ecg-but.html ) — and if you've not seen the neat little article by Rowlands and Moore on this subject — Figures 2,3,4 in this Sept. 27 Blog post reproduce their article that reviews specific lead derivations (I LOVE their little article! — :) — And while I AGREE with your reasoning for determining the "culprit extremity" causing the artifact — ECG #1 (in my Figure-1) shows a bit more prominent artifact for the 1st beat in aVR than I would have expected with the left Foot as the source ... Otherwise, if one accepts my premise that ALL beats "A" in ECG #1 are influenced by artifact — then there were not marked abnormalities (beyond hyperacute T waves in V2,V3) on that initial ECG — so reperfusion changes (T wave inversion) might not yet be forthcoming (as they were later on). THANKS again for your comments! — :)
DeleteTo Dr. Ken Grauer:
ReplyDeleteGreat point about artifact distorting ECG 1, - I was reading this post from my phone and didn't notice this beat-to-beat difference, interpreting ECG looking at first beats only.
About that strange artifact pattern: this is explained by operation mode of ECG recorder: it records all 12 leads simultaneously and prints same 2,5 seconds of recording but from different leads. Labeling on top confirms that - 2,5-5,0 seconds are used every time. So it's a single artifact repeated over and over.
Thanks for a good analysis.
@ Max Romanchenko — THANK YOU Max! — :)
Delete