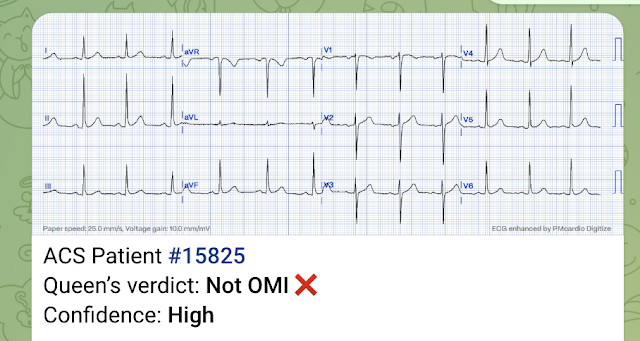
A 50-something woman with history of DM and HTN presented with one hour of chest tightness. I was screening all patients at triage and we obtained this ECG:
I was worried about the small amount of ST elevation in inferior leads, with a bit of reciprocal STD in aVL.
There is also T-wave inversion in V2, which is usually a very suspicious sign of early posterior MI. Posterior MI of course is strongly associated with inferior MI. However, the P-wave in V2 is inverted, which tells us that the lead was placed too high and this usually results in false positive T-wave inversion in V2.
So I was not entirely convinced.
 |
| The computer read was "Normal ECG" What do you think? Veritas algorithm |
I was worried about the small amount of ST elevation in inferior leads, with a bit of reciprocal STD in aVL.
There is also T-wave inversion in V2, which is usually a very suspicious sign of early posterior MI. Posterior MI of course is strongly associated with inferior MI. However, the P-wave in V2 is inverted, which tells us that the lead was placed too high and this usually results in false positive T-wave inversion in V2.
So I was not entirely convinced.
the Queen of Hearts has mid confidence:
A previous ECG was available from a few months prior:
 |
| This also had some inferior STE, but with less STD in aVL |
The Queen knows that this basline (above) is not OMI:
Let's look at the limb leads side-by-side:
I did not think it diagnostic, but wrote in my triage note:
"ECG equivocal and will need frequent serial ECGs."
The ED was incredibly busy, with 40 patients waiting in triage for beds (all of whom I had already screened), so we put her in a chair in triage. The wait for a bed was approximately 4 hours.
I went back to screening patients and time flew by and I forgot to get the 15 minute follow up ECG, but then remembered and did get one at about 45 minutes:
My interpretation: This is a clear change and diagnostic of inferior MI.
I activated the cath lab and brought her to the critical care area.
While the cath lab was getting ready, we recorded a right sided ECG:
Angiogram showed a distal RCA occlusion which was stented.
Echo showed inferior wall motion abnormality.
If in our system we did not interrupt physicians with "normal" ECG, this OMI would have been completely missed, even with 2 ECGs! And she would have waited 4 hours in triage while her myocardium infarcted.
This probably happens frequently. We know that 25% of OMI do not get emergent angiography. Many of them might be sitting in triage.
Learning Points:
The computer cannot be trusted when it says "Normal ECG"
The triage physician should see every ECG, but this only helps if the triage physician can recognize MI that the computer does NOT recognize (i.e., many readers of this blog).
 |
| Again, the major difference is the slightly greater ST depression in aVL If I would follow my own rules, I would have diagnosed acute MI earlier. |
I did not think it diagnostic, but wrote in my triage note:
"ECG equivocal and will need frequent serial ECGs."
The ED was incredibly busy, with 40 patients waiting in triage for beds (all of whom I had already screened), so we put her in a chair in triage. The wait for a bed was approximately 4 hours.
I went back to screening patients and time flew by and I forgot to get the 15 minute follow up ECG, but then remembered and did get one at about 45 minutes:
 |
| Computer interpretation: "Normal ECG" Veritas algorithm again What do you think? The Queen knows this one too: |
My interpretation: This is a clear change and diagnostic of inferior MI.
I activated the cath lab and brought her to the critical care area.
While the cath lab was getting ready, we recorded a right sided ECG:
 |
| V1=V1R which is the same location as V2 V2 = V2R = same location as V1 V3-V6 = V3R - V6R Inferior MI is obvious There is no right ventricular MI evident on these ECGs. |
Angiogram showed a distal RCA occlusion which was stented.
Echo showed inferior wall motion abnormality.
If in our system we did not interrupt physicians with "normal" ECG, this OMI would have been completely missed, even with 2 ECGs! And she would have waited 4 hours in triage while her myocardium infarcted.
This probably happens frequently. We know that 25% of OMI do not get emergent angiography. Many of them might be sitting in triage.
Learning Points:
The computer cannot be trusted when it says "Normal ECG"
The triage physician should see every ECG, but this only helps if the triage physician can recognize MI that the computer does NOT recognize (i.e., many readers of this blog).
-----------------------------------------------------------
Comment by KEN GRAUER, MD (9/11/2018):
-----------------------------------------------------------
The lesson in this case relates to the recognition of subtle abnormalities that typically go undetected by the computerized interpretation — and which also may be overlooked by clinicians in the setting of a busy ED. Dr. Smith expertly highlights the subtle findings in this case that caught his eye. My comments address a few additional differences between the 3 ECGs that were done in this case — with focus on how to put the subtleties I describe in perspective in view of the overall picture (Figure-1).
- I’ll emphasize that much of what I write below IS painstakingly detailed beyond the usual description. My purpose in doing so is my belief that awareness of these subtleties is what distinguishes the astute ECG diagnostician from his/her peers.
 |
| Figure-1: Comparison of the 3 ECGs in this case (See text below). |
---------------------------------------
ECG #1 — obtained from this 50yo woman who presented with 1 hour of chest tightness:
- As per Dr. Smith — the worrisome findings include suggestion of slight ST elevation in each of the inferior leads that occurs in association with subtle-but-real mirror-image ST depression in lead aVL (For review of what I mean by “mirror-image” ST depression — CLICK HERE and scroll down to My Comment).
- The presence of artifact should be noted in ECG #1. This is most pronounced in leads I, II; aVR, aVL, and aVF. There are times when the presence of artifact impedes accurate interpretation. That said, it should be recognized in this case that despite the artifact — the shape of the ST-T wave in lead aVL is unmistakably abnormal in each of the 3 beats in this lead. This is the reason for Dr. Smith’s initial concern.
- There is slight variation in QRS amplitude in several of the beats in the limb leads. This phenomenon commonly arises because of respiratory variation that is often seen in acute patients. It is important to recognize — because sometimes both Q waves and ST-T wave changes may differ from beat-to-beat. That said, despite the differences in the QRS complex in lead aVL of ECG #1 (ie, the first QRS is isoelectric, whereas the next 2 complexes are predominantly positive) — the abnormal ST depression in lead aVL persists in all 3 beats in this lead. We therefore assume this is a real finding.
- The common reasons for P wave negativity in lead V1 are LAA (Left Atrial Abnormality), atrial conduction defects, and lead placement 1 or 2 interspaces too high on the chest. The reason: we KNOW in ECG #1 that the leads were placed too high on the chest for both leads V1 and V2 are: i) the QRS complexes in leads aVR, V1 and V2 all look the same (ie, a virtually all negative QRS complex with T wave inversion); ii) the P wave in leads V1 and V2 is all negative, with a surprisingly deep negative component; and iii) there is fairly abrupt transition from these identical-looking QRST complexes in leads V1,V2 — to an already isoelectric QRS with tall positive T wave by lead V3. This is relevant — because it tells us we have NO idea what a “real V1 and V2” would look like. Therefore, we are handicapped by not being able to assess whether changes are present that might suggest ongoing posterior infarction. But even if the T wave inversion in V1,V2 was real — acute posterior infarction most often is associated with J-point ST depression in anterior leads with a picture of the ST segment that is the mirror-image of inferior ST elevation. Symmetric T wave inversion as seen in ECG #1 may be ischemic — but is less often associated with acute evolving posterior infarction.
ECG #2 — which is a “baseline” tracing done a few months earlier.
- As per Dr. Smith — there is a change in the ST-T wave appearance in lead aVL of ECG #1, compared to what aVL looked like in this baseline tracing. This change in appearance adds to our suspicion that something acute is going on.
- Again, it should be noted that there are slight differences from one beat to the next in lead aVL (ie, Note predominant negativity for the 3rd beat in this lead in ECG #2) — and, that there is slight change in the frontal plane axis between the 2 tracings (ie, the axis in ECG #2 is now clearly closer to +60 degrees). While I’ll emphasize that these findings do not alter our impression that there is new ST depression in lead aVL of ECG #1 — My point is merely to point out that the astute ECG diagnostician needs to take into account even slight differences in beat-to-beat QRS morphology, as well as any change in frontal plane axis, as part of the overall process for determining which findings may or may not impede accurate lead-to-lead comparison of tracings.
- Note in ECG #2 (= the “baseline” tracing from a few months earlier) — that a more normal appearance was present in leads V1 and V2. That is, the P wave in lead V1 in ECG #2 was biphasic, and predominantly positive in V2 — the T wave in V1 is less deeply inverted, and now all positive in V2 — and R wave progression was normal without abrupt transition. To me, this confirms that leads V1 and V2 in ECG #1 were indeed placed too high on the chest ...
ECG #3— obtained 45 minutes after ECG #1.
- As per Dr. Smith — ECG #3 is now clearly diagnostic of acute inferior OMI. Note again (compared to ECG #1) — the more normal appearance in ECG #3 of P wave morphology in V1 and V2, with normal R wave progression in the chest leads (albeit still with no indication of acute posterior infarction).
Our thanks to Dr. Smith for this superb teaching case!



No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.