This male in his 40's had been having intermittent chest pain for one week. He awoke from sleep with crushing central chest pain and called ems. EMS recorded a 12-lead, then gave 2 sublingual nitros with complete relief of pain. He arrived in the ED and had this ECG recorded:
When the patient had chest pain, prior to nitroglycerine, what do you think the ECG showed? See below.
Here is the prehospital ECG, with pain:
 |
| Hyperacute anterolateral STEMI |
The medics had activated the cath lab and the patient went for angiogram and had a 95% stenotic LAD with TIMI-3 flow. A stent was placed.
Here is the 3 hour post angio ECG:
 |
| The Wellens' waves are receding (this is unusual) |
The next AM, another ECG was recorded:
A transthoracic echo done next day was entirely normal. The peak troponin I was 0.364 ng/ml.
The reperfusion was so early that wall motion recovered completely and early.
For those who depend on echocardiogram to confirm the ECG findings of ischemia, this should be sobering. I have seen cases of Wellens' syndrome that were ignored because of either negative troponins or normal echo or both and the patient did not get an angiogram and had a bad outcome.
Wellen's syndrome is a Reperfusion syndrome. All of Wellens' cases in his studies (1, 2) had all of:
1) preserved R-waves
2) resolution of pain
3) restored flow to the anterior wall through either
a) an open artery or
b) collateral circulation.
This is a rare case in which we can prove that the Wellens' waves represent spontaneous reperfusion because we recorded a prehospital ECG during pain. Such a mechanism is supported by the work of Doevendans (3) and Wehrens (4), who both described terminal T-wave inversion (which have the same morphology as Wellens' waves) as the earliest sign of reperfusion from reperfusion therapy. (I don't know that this connection has ever been formally written about in any original literature, though I have long maintained that this is the pathophysiology of Wellens' waves.)
In my experience, all Wellens' with significant myocardial infarction have evolution from type A waves to type B waves over 6-24 hours' time, so that the presence of type A or type B waves, I believe, are simply a matter of the timing of recording and the rapidity of evolution. In this case, the duration of ischemia was so brief that there was no such evolution, and there was near-normalization. When there is extremely brief ischemia, as in this case, or this case, it may entirely reverse, especially in unstable angina (negative troponins).
Lessons:
1. Wellens' syndrome represents a state of reperfusion of the infarct related artery
2. Ischemia may be so brief that Wellens' waves do not evolve
3. Ischemia may be so brief that troponins are borderline or normal
4. Ischemia may be so brief that wall motion normalizes (though presence of wall motion abnormality would have a very high positive predictive value for confirming the ECG findings.).
1. de Zwaan C., Bar F.W., Janssen J.H.A., et al. Angiographic and clinical characteristics of patients with unstable angina showing an ECG pattern indicating critical narrowing of the proximal LAD coronary artery. Am Heart J (1989) 117 : pp 657-665.
2. de Zwaan C., Bar F.W., Wellens H.J.J., Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J (1982) 103 : pp 730-736. 3. Doevendans P.A., Gorgels A.P., van der Zee R., et al. Electrocardiographic diagnosis of reperfusion during thrombolytic therapy in acute myocardial infarction. Am J Cardiol (1995) 75 : pp 1206-1210.
4. Wehrens X.H., Doevendans P.A., Ophuis T.J., et al. A comparison of electrocardiographic changes during reperfusion of acute myocardial infarction by thrombolysis or percutaneous transluminal coronary angioplasty. Am Heart J (2000) 139 : pp 430-436.
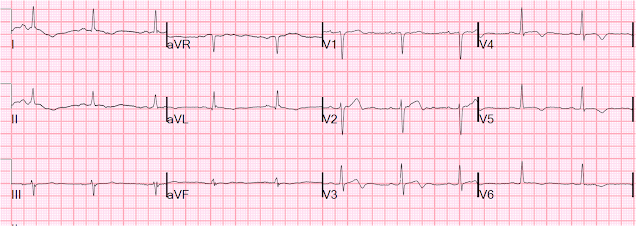 |
| The Wellens' waves are still present, and not evolving |
The reperfusion was so early that wall motion recovered completely and early.
For those who depend on echocardiogram to confirm the ECG findings of ischemia, this should be sobering. I have seen cases of Wellens' syndrome that were ignored because of either negative troponins or normal echo or both and the patient did not get an angiogram and had a bad outcome.
Wellen's syndrome is a Reperfusion syndrome. All of Wellens' cases in his studies (1, 2) had all of:
1) preserved R-waves
2) resolution of pain
3) restored flow to the anterior wall through either
a) an open artery or
b) collateral circulation.
This is a rare case in which we can prove that the Wellens' waves represent spontaneous reperfusion because we recorded a prehospital ECG during pain. Such a mechanism is supported by the work of Doevendans (3) and Wehrens (4), who both described terminal T-wave inversion (which have the same morphology as Wellens' waves) as the earliest sign of reperfusion from reperfusion therapy. (I don't know that this connection has ever been formally written about in any original literature, though I have long maintained that this is the pathophysiology of Wellens' waves.)
In my experience, all Wellens' with significant myocardial infarction have evolution from type A waves to type B waves over 6-24 hours' time, so that the presence of type A or type B waves, I believe, are simply a matter of the timing of recording and the rapidity of evolution. In this case, the duration of ischemia was so brief that there was no such evolution, and there was near-normalization. When there is extremely brief ischemia, as in this case, or this case, it may entirely reverse, especially in unstable angina (negative troponins).
Lessons:
1. Wellens' syndrome represents a state of reperfusion of the infarct related artery
2. Ischemia may be so brief that Wellens' waves do not evolve
3. Ischemia may be so brief that troponins are borderline or normal
4. Ischemia may be so brief that wall motion normalizes (though presence of wall motion abnormality would have a very high positive predictive value for confirming the ECG findings.).
1. de Zwaan C., Bar F.W., Janssen J.H.A., et al. Angiographic and clinical characteristics of patients with unstable angina showing an ECG pattern indicating critical narrowing of the proximal LAD coronary artery. Am Heart J (1989) 117 : pp 657-665.
2. de Zwaan C., Bar F.W., Wellens H.J.J., Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J (1982) 103 : pp 730-736. 3. Doevendans P.A., Gorgels A.P., van der Zee R., et al. Electrocardiographic diagnosis of reperfusion during thrombolytic therapy in acute myocardial infarction. Am J Cardiol (1995) 75 : pp 1206-1210.
4. Wehrens X.H., Doevendans P.A., Ophuis T.J., et al. A comparison of electrocardiographic changes during reperfusion of acute myocardial infarction by thrombolysis or percutaneous transluminal coronary angioplasty. Am Heart J (2000) 139 : pp 430-436.


Great case! Thank you for this one.
ReplyDeleteI must admit that I was half expecting de Winter T waves when I read the question about prehospital ecg (before I actually looked at it) :-). But this was equally interesting..
Steve
ReplyDeleteA new or indeterminate echocardiographic RWMA in a region of normal thickness myocardium should be regarded a good positive predicative value. Your case speaks to less than perfect neg predictive value of the echo, I agree with that.
Absolutely. A wall motion abnormality would confirm Wellens'. Good PPV.
ReplyDeleteFurthermor, absence of wall motion abnormality at the time of ED presentation would have a very high negative predictive value. But this one was done after the angiogram.
I can imagine that if no prehospital ECG had been done, the patient could have been admitted and because of a normal echo, not had an angiogram. I have seen this happen, even with a positive troponin.