Written by Willy Frick
A 50 year old man with no medical history presented with acute onset substernal chest pain. His ECG is shown below.
Pretty obvious anterior current of injury. This was a machine read STEMI positive OMI. Readers of this blog can easily appreciate the hyperacute T waves in the precordium, clearest in V1-V4.
What would you guess is the culprit artery?
Angiography is shown below
This is right anterior oblique caudal
Here is a representative still. This shot is typically best for viewing the LAD and its diagonal branches. The LCx and OM branches are not as well seen. There is non-obstructive disease here.
This is the stump that remains of the RCA.
How does RCA occlusion fit with the ECG?
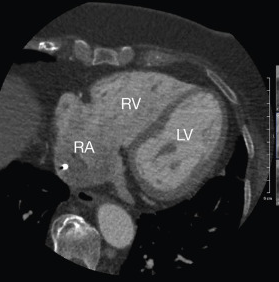
The answer is that the ECG really shows right ventricular OMI. Remember that the RV is the most anterior chamber. Here is a transverse image of a CT showing this.
In this patient's case, the RV ischemia manifested as dramatic anterior hyperacute T waves. A few clues that might have suggested this are:
- There is marked STE in V1. This degree of STE is a bit atypical for LAD ischemia. If it happens, you might expect to see lateral precordial STD -- the precordial swirl pattern.
- There is no clear involvement in the high lateral leads or the lateral preocordial leads. It's a predominantly anterior and rightward current of injury.
- There is a very good sized R wave in V4. LAD OMI typically causes some diminution in the V4 R wave.
In this patient's case, the answer was clear at time of angiography, but the "culprit game" is more important than just a fun parlor trick. In this important paper (DOI: 10.1161/CIRCINTERVENTIONS.118.007305) from Heitner et al., the investigators reviewed outcomes in 118 patients presenting with NSTEMI. All patients underwent cardiac magnetic resonance imaging to determine the precise location of infarct. The whole paper is astonishing, but among other things, the investigators found:
- 31% of patients had a misidentified infarct related artery from angiography
- 15% of patients had altogether non-ischemic pathogenesis, despite being clinically adjudicated as NSTEMI
- The above two groups comprised 46% of patients in the study
- Of the patients who underwent revascularization, 27% received PCI exclusively to non-culprit arteries
In other words, in patients who lack STEMI criteria, angiography performs exceptionally poorly in identifying the problem. It is easy to see how this could include patients with reperfused or subtle OMI patterns.
Imagine if the patient in this had a bystander severe stable proximal LAD lesion, and imagine if he had spontaneously reperfused the culprit artery. It is easy to imagine he could have had PCI to the wrong vessel. Thankfully that did not occur. Even if it might be challenging to suspect prospectively, it is important to understand why the angiography is not surprising at all.
Learning points:
- RV OMI can manifest with an anterior current of injury
- Suspect RV involvement when there is pronounced STE in V1
- It is important to at least have a reasonable guess as to the most likely culprit for an MI
See this case:
Right Ventricular MI seen on ECG helps Angiographer to find Culprit Lesion
===================================
MY Comment, by KEN GRAUER, MD (8/2/2024):
===================================
Among the many famous quotes of the great fictional detective Sherlock Holmes, is the following — "There is nothing more deceptive than an obvious fact" (from Sir Arthur Conan Doyle's book = "The Boscombe Valley Mystery", 1891).
- The meaning of this quote is that at times, something as obvious as the dramatic anterior lead ST elevation that we see in today's tracing is not the result of an acute LAD STEMI.
- The problem with jumping ahead and immediately accepting such seemingly "obvious facts" — is that this predisposes to premature closure without fully considering other diagnostic possibilities — which in this case should include acute proximal RCA occlusion, with resultant RV MI as the cause of the marked anterior ST elevation.
- We need the self-discipline of a Sherlock Holmes, who refrained from jumping to conclusions — and instead, always remained open to other possibilities.
KEY Point: Acute RV MI is easy to overlook — simply because it is a much less common cause of acute anterior ST elevation than acute LAD occlusion. Yet recognition of acute RV MI is extremely important clinically — because emergency treatment will often require different priorities (ie, avoidance of nitroglycerine; fluid resuscitation for hypotension).
- We've highlighted a considerable number of acute RV MI cases in Dr. Smith's ECG Blog (See the October 7, 2019 and May 10, 2024 posts, to name just two). It's much easier to think about the possibility of acute RV MI in cases like these — in which there is inferior lead ST elevation and less marked anterior ST elevation that is not nearly as extensive as seen in today's case.
- It's much more challenging to consider acute RV MI from an ECG like the one in today's case (that I've reproduced in Figure-1) — in that the seemingly obvious fact of "eye-catching" ST elevation in leads V1-thru-V4 (nearly 10 mm of ST elevation in lead V2!) — encourages a conclusion of acute LAD occlusion.
- When inferior lead ST elevation is present — ordering right-sided leads is extremely helpful for localizing acute RCA OMI to a proximal site in this artery, that confirms RV MI when right-sided ST elevation is seen (See My Comment in the July 19, 2020 and May 30, 2023 posts). But in the face of marked anterior ST elevation — there is no inferior lead ST elevation in Figure-1 (within the BLUE rectangles), therefore deceptive in leading the clinician away from considering acute RV involvement.
PEARL #1: The important paper cited by Dr. Frick in his discussion above (Heitner et al — Cardiovasc Interven 12(5), 2019) — highlights the fact that learning to predict the probable "culprit" artery from interpretation of the initial ECG is more than simply an academic exercise.
- Regardless of what the "culprit" artery in today's case turned out to be — the need for cardiac cath was immediately obvious from the marked anterior ST elevation in Figure-1. But as per Dr. Frick — it could have been easy to overlook the RCA culprit in today's case IF, for example — that vessel had spontaneously reperfused and the patient had an incidental stable LAD narrowing that was not the culprit in today's event.
- The above noted article by Heitner et al, makes the important point that cardiac cath fails to correctly identify the "culprit" artery in a significant percentage of patients, especially in patients with acute OMI in the absence of frank ST elevation. Getting good at predicting the likely "culprit" artery can assist the interventionist by suggesting where to look for evidence of which artery caused the infarct.
PEARL #2: I'll emphasize another point highlighted by Dr Frick in his discussion — namely, that despite ST elevation in leads V1-thru-V4 — there are clues in Figure-1 that the "culprit" artery is not the LAD:
- Chest lead ST elevation that begins (and is already marked) in lead V1, attaining the huge amplitude of ST elevation that we see in lead V2 of today's case — usually indicates proximal LAD occlusion.
- But in such proximal LAD occlusions — there is almost always significant ST elevation in lead aVL. However — no ST elevation at all is seen in lead aVL in Figure-1 (within the RED rectangle).
- Although inferior lead reciprocal ST depression is not always seen with LAD OMI — it usually is seen when the site of acute LAD occlusion is proximal. But considering the amount of anterior lead ST elevation in Figure-1 — the amount of inferior lead ST depression is less than I would expect if there was proximal LAD occlusion.
- Finally (as per Dr. Frick) — given the shape and amount of ST elevation in lead V1, I would expect more ST elevation in lead aVR, and more reciprocal ST depression in lead V6 if the cause of anterior ST elevation was "Swirl" from the septal ischemia of a very proximal LAD occlusion (See My Comment in the October 15, 2022 post on Precordial Swirl).
BOTTOM Line: Remember that in addition to LAD OMI — acute RV MI is another less common but very important cause of anterior ST elevation.
- IF you are considering acute RV MI in the patient in front of you — obtaining right-sided leads can quickly confirm your suspicion.
- In the absence of inferior lead ST elevation — the clues provided in PEARL #2 suggest right-sided leads are still worthwhile to rule in or out acute RV MI.
-USE.png) |
| Figure-1: The initial ECG in today's case — with attention to the art of considering all possibilities à la Sherlock Holmes. (To improve visualization — I've digitized the original ECG using PMcardio). |




No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.