Written by Willy Frick
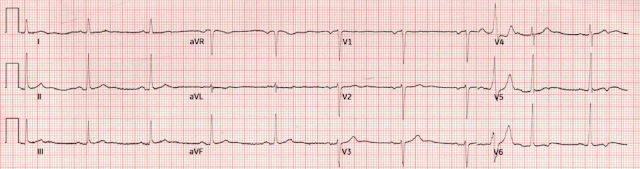
A man in his early 40s with BMI 36, hypertension, and a 30 pack-year smoking history presented with three days of chest pain. It started while he was at rest after finishing a workout. He described it as a mild intensity, nagging pain on the right side of his chest with nausea and dyspnea. It woke him the next day and radiated into his back. He was only able to sleep while sitting in a chair. He went to urgent care and had an ECG (not available) which was interpreted as normal, and was sent home. His pain returned, and he went back to the urgent care but was sent to the ER. His ECG is shown:
What do you think?
Here is the Queen's verdict and translator:
For me, it is hard to make much of this ECG. The most troublesome lead is aVL which shows abnormal ST flattening and perhaps even a very tiny of depression. With no context, I would call it sinus rhythm with non-specific ST&T wave abnormalities.
Smith: there is a bit of STE in inferior leads, and aVL has not only some STD, but it is downsloping, which is very worrisome for inferior OMI.
High sensitivity troponin I (hsTnI) obtained around that time was 5548 ng/L (ref. < 35). This is enough to cause serious alarm. Distilling this case into its most salient components, a man with multiple risk factors for coronary disease is presenting with several days of chest pain and markedly elevated troponin with no other reason to explain the lab abnormality (e.g. sepsis). It is impossible to overstate the importance of putting the ECG and troponin into the context of the clinical history.
Smith: at this point, the ECG becomes irrelevant. The patient has ACS by history, active pain, and an elevated troponin. There is acute MI with persistent symptoms. This is an indication for the cath lab regardless of the ECG. Nevertheless, learning these ECGs is critical because the next time such a patient presents, it might be acute, before there is any troponin elevation. Activate the cath lab! Do not wait for repeat troponins or ECGs.
Already, we should be asking ourselves whether this could be OMI. And since the ECG does not define the disease, the answer is of course it could be. Troponin is not specific for acute coronary syndrome, but in a case like this when we have nothing else to explain it, we must rule out the deadliest (reasonably likely) possibility. Repeat ECG was obtained and is shown below:
Here is the Queen's verdict and translator:
I sent these ECGs along with the troponin trend to our group chat, and Dr. Nossen said "With those troponins retrospectively, this is an inferoposterior OMI. It would be hard to call without the previous ECG for comparison, but the inferior leads are worrisome." Dr. Hellerman agreed and mentioned the inferior ST elevations with reciprocal depression in aVL. Dr. Smith (catching up on the discussion) saw ECG 1 and commented that it looked like "very subtle inferior OMI."
Dr. Nossen also pointed out that with voltage this high in the limb leads, you would typically expect some degree of inferior/inferolateral ST depression (the so-called "LVH strain" pattern), and in fact this patient did have severe LVH on subsequent echocardiogram (which Dr. Nossen did not know at the time). Therefore, the finding of any STE inferiorly is doubly alarming.
Here they are side by side:
The T waves in the inferior leads have significantly increased in volume, and the mostly flat ST segment in aVL now has more of a down-up morphology.
Around this time, the patient received aspirin 324 mg. Repeat hsTnI was 10497 ng/L, and this was interpreted as "likely NSTEMI." Note that this patient has elevated troponin with dynamic change and chest pain. By definition, this is acute myocardial infarction, the only question now is the etiology.
Given radiation of pain into the patient's back, he underwent CTA which showed no evidence of aortic dissection or any other acute pathology. It is not clear exactly what symptoms the patient may have been experiencing at this time, but the notes indicate that he then developed "worsening" pain, suggesting he had likely had ongoing angina the whole time. Recall that medically refractory angina is itself a Class I indication for immediate angiography (see Figure 8). (It is hard to call this medically refractory at this point as the patient had not received any anti-anginal therapy.)
At this point, the patient was treated with 1 inch of nitro paste (Smith: this is a worthless treatment and the ACC guidelines even say so!) and morphine 4 mg IV (Smith: this is even more worthless, and just hides the fact that the patient is having ongoing ischemia and infarction), and repeat ECG was obtained. (Treating angina with morphine and continuing non-emergent management is like taking the batteries out of an actively alarming smoke detector during a house fire and going back to sleep.)
Another ECG was recorded:
Here is the Queen's verdict and translator:
Compared to the first two ECGs, and especially in the context of chest pain and rapidly rising troponin, we see progressively increasing area under the curve in the inferior T waves, and the ST segment in aVL now has much clearer reciprocal depression.
A third hsTnI was 17809 ng/L, and the patient was started on IV heparin as well as sublingual and IV nitroglycerin. Due to persistent pain, he received a second dose of morphine 4 mg IV. Repeat hsTnI was 25763 (ten hours after the initial result).
Brief aside: Remember that the overwhelming benefit of reperfusion therapy is attained if performed within 2-3 hours. By 6 hours, most of the salvageable myocardium has infarcted. This is WHY refractory angina should prompt immediate angiography. If you wait until the ECG and troponin are "convincing," you are sacrificing a lot of myocardium.
Due to persistent pain, the patient received a third dose of morphine 4 mg IV. A fourth ECG is shown below.
Here is the Queen's verdict and translator:
If any doubt remained, we are now completely certain that the inferior T waves are hyperacute, especially with the reciprocal changes in aVL. Although this ECG is obvious to the Queen of Hearts, it was read by cardiology as sinus rhythm with non-specific ST&T wave abnormality.
At this point, due to refractory pain, the patient was taken for left heart catheterization. It is not clear why it was only considered refractory after topical, sublingual, and intravenous nitroglycerin plus morphine 12 mg IV over the course of over 10 hours. But unfortunately, this is not surprising, only about 6% of patients with refractory angina receive immediate angiography as recommended.
Thirteen hours after the first troponin was drawn, the following angiogram was performed.
The troponin peaked at 25749 ng/L. Echocardiogram showed akinesis of the mid to basal inferior and inferoseptal walls, and hypokinesis of the inferolateral wall. One final ECG performed after cath shows obvious inferoposterior reperfusion. (Deep TWI in the inferior leads with reciprocal overly upright T waves in I and aVL, plus posterior reperfusion T waves in V1-2 at least.)

False negative by Queen of Hearts: All ECGs like this will be reviewed in detail by Powerful Medical, and these "critical misses" will be rectified in the algorithm!
The Queen of Hearts PM Cardio App is now available in the European Union (CE approved) the App Store and on Google Play. For Americans, you need to wait for the FDA. But in the meantime:
YOU HAVE THE OPPORTUNITY TO GET EARLY ACCESS TO THE PM Cardio AI BOT!! (THE PM CARDIO OMI AI APP)
If you want this bot to help you make the early diagnosis of OMI and save your patient and his/her myocardium, you can sign up to get an early beta version of the bot here. It is not yet available, but this is your way to get on the list.
Learning points:
- ECG owes you nothing in OMI, and may be completely normal, or show only impossibly subtle findings.
- Fortunately, ECG is not the only diagnostic information to clue you into the possibility OMI! There is history, physical, troponin, and bedside echo.
- There are many causes of elevated troponin, but unexplained troponin elevation in a patient with ongoing chest pain is OMI until proven otherwise.
- Patients with medically refractory angina should undergo immediate angiography.










No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.