Acute coronary syndrome in a pediatric patient?
Written by Kirsten Morrissey, MD with edits by Bracey,
Grauer, Meyers, and Smith
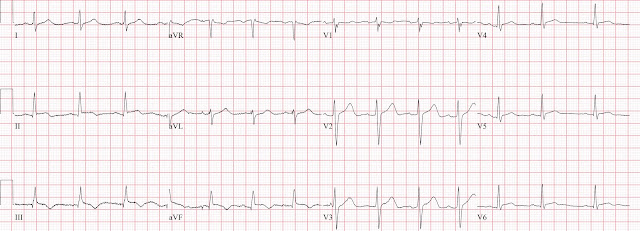
An older teen was transferred from an outside hospital with elevated serum troponin and and ECG demonstrating ST elevations.
The patient was obese and had a medical history of only recurrent tonsillitis status post tonsillectomy and adenoidectomy but was otherwise healthy and fully vaccinated. He reported 1.5 days of chest pain that started as substernal and crushing in nature awakening him from sleep and occasionally traveling to right side of neck. The pain was described as constant, worse with deep inspiration and physical activity, sometimes sharp. Reports occasional dizziness but no syncope, no recent illness, no recent fever, no trauma, no tick bites, no lower extremity swelling, no viral symptoms. He denied drug or alcohol use. He did have a family history notable for early CAD.
 |
| NSR with ST elevation II,III, aVF with reciprocal depression in aVL |
Would you refer this pediatric patient for emergent PCI?
The workup at the transferring hospital yielded elevated troponin I at 18.1 ng/mL (ULN <0.01), borderline elevated D-dimer at 0.56 mgL, without any clinical evidence of an infectious process. Serum WBC and CRP, platelet count were within normal limits, negative respiratory viral panel, and chest XR revealed no acute findings and normal heart size and cardiac silhouette. The ECG performed at the referring facility was reported to have ST elevations in leads II,III and aVF.
On arrival, the patient had normal vital signs (including temperature) and appeared overall well, if a bit anxious, and still reporting intermittent chest pain and heaviness.
31 Year Old Male with RUQ Pain and a History of Pericarditis. Submitted by a Med Student, with Great Commentary on Bias!
A teenager with chest pain, a troponin below the limit of detection, and "benign early repolarization"
Smith sent this ECG to the PM Cardio Queen of Hearts AI system and this was the response:
The Queen of Hearts PM Cardio App is now available in the European Union (CE approved) the App Store and on Google Play.
For Americans, you need to wait for the FDA. But in the meantime:
Case Continued
Repeat labwork revealed a high sensitivity troponin I result of >16,000 ng/L, mildly elevated CRP of 8.4 mg/L and a normal WBC of 8.8. Pediatric cardiology performed a bedside echo in ED with EF estimation of 60%, no pericardial effusion, and no regional wall motion abnormalities.
A repeat ECG was performed as adult cardiology was asked to evaluate the patient for emerget PCI:
 |
| Sinus bradycardia with persistent elevation in the inferior leads with reciprocal depression in aVL |
Patient was taken to cath lab with adult cardiology which revealed normal coronary arteries without evidence of occlusion MI.
Smith: this was the prudent thing to do!!
He was started on colchicine for presumed myocarditis and discharged after a brief, uneventful hospital course.
A final ECG was perfomed on hospital day 2:
 |
| Persistent ST elevation in the inferior leads with slight reciprocal ST depression in aVL |
Teaching points
- It is essential to consider ACS in all age groups. Though less prevalent in younger patients, occlusion MI may occur and requires the same early interventions as older patients.
- - Pericarditis and myocarditis should be a diagnosis of exclusion. Eleveated serum troponin levels and ST changes, particularly though in anatomical distributions by ECG, should be considered OMI until proven otherwise.
rs.- While ACS may be less common in the pediatric population, it is important to consider risk factors that may make OMI more likely (e.g., hematological disorder like sickle cell or antiphospholipid syndome, family history of CAD or hypercholesterolemia, prior history of vasculopathies such as Kawasaki Disease, MIS-C, prior cardiac surgery, etc.)
References
Law YM, Lal AK, Chen S, Čiháková D, Cooper LT
Jr, Deshpande S, Godown J, Grosse-Wortmann L, Robinson JD, Towbin JA; American
Heart Association Pediatric Heart Failure and Transplantation Committee of the
Council on Lifelong Congenital Heart Disease and Heart Health in the Young and
Stroke Council. Diagnosis and Management of Myocarditis in Children: A
Scientific Statement From the American Heart Association. Circulation. 2021 Aug
10;144(6):e123-e135. doi: 10.1161/CIR.0000000000001001. Epub 2021 Jul 7. Erratum
in: Circulation. 2021 Aug 10;144(6):e149. PMID: 34229446.
Newburger JW, Takahashi M, Burns JC. Kawasaki
Disease. J Am Coll Cardiol. 2016 Apr 12;67(14):1738-49. doi:
10.1016/j.jacc.2015.12.073. PMID: 27056781.
Silva Andrade B, Siqueira S, de Assis Soares
WR, de Souza Rangel F, Santos NO, Dos Santos Freitas A, Ribeiro da Silveira P,
Tiwari S, Alzahrani KJ, Góes-Neto A, Azevedo V, Ghosh P, Barh D. Long-COVID and
Post-COVID Health Complications: An Up-to-Date Review on Clinical Conditions
and Their Possible Molecular Mechanisms. Viruses. 2021 Apr 18;13(4):700. doi:
10.3390/v13040700. PMID: 33919537; PMCID: PMC8072585.
Zhang QY, Xu BW, Du JB. Similarities and
differences between multiple inflammatory syndrome in children associated with
COVID-19 and Kawasaki disease: clinical presentations, diagnosis, and
treatment. World J Pediatr. 2021 Aug;17(4):335-340. doi: 10.1007/s12519-021-00435-y.
Epub 2021 May 20. PMID: 34013488; PMCID: PMC8134825.
MY Comment, by KEN GRAUER, MD (12/5/2023):
- While an older teen who is overweight will generally manifest similar ECG criteria as an adult — today's case nevertheless raises the question of WHAT are potential etiologies of an acute MI in a pediatric patient?
- By way or review in Figure-2 — I've developed a list of potential causes of acute MI to consider in the pediatric age group.
- Ultimately, cardiac cath was done — revealing patent coronary arteries. That said — I'd add the following to the discussion by Drs. Morrissey and Bracey regarding subtle hints that today's initial ECG (that I've labeled in Figure-1) was more suggestive of acute myocarditis than OMI.
- STATISTICS — Namely, that in the previously healthy teenage/young adult age group, acute myocarditis is much more common than acute infarction. That said — acute MI does occasionally occur in these younger patients, so statistics alone do not suffice to rule out this possibility.
- NOTE: We've shown on a number of occasions in Dr. Smith's ECG Blog how difficult it may sometimes be to distinguish between acute myocarditis vs acute OMI on the basis of ECG findings and the clinical history (See My Comments in the July 21, 2019 — December 10, 2019 — April 25, 2023 — December 31, 2019 — and January 10, 2020 posts).
- Given ST elevation in the 3 inferior leads — the finding of more ST elevation in lead II > III — would suggest a LCx (rather than RCA) "culprit". If this were the case — I would typically expect high-lateral ST elevation, rather than the peaked T wave with isoelectric ST segment in lead I (BLUE arrow in this lead) — with isoelectric ST segment in lead aVL.
- The peaked T waves in leads I and II (without hint of even an upright T in lead III) — is clearly more suggestive of pericarditis/myocarditis, than of an acute OMI (ie, Lead II tends to resemble lead I more than lead III with pericarditis).
- Most of the time with a LCx culprit — there will be evidence of associated posterior OMI — but the ST segments in leads V2,V3 are upward-sloping and slightly elevated rather than depressed (RED arrows in these leads).
- In fact — there is J-point ST elevation in 5 of 6 chest leads (ie, in leads V2-thru-V6), a finding much more consistent with pericarditis/myocarditis than acute OMI (especially given what appears to be an elevated ST/T wave ratio in lead V6).
- The ST segment in lead aVL is no more than minimally depressed — which I would not expect given the lack of any ST elevation in the other high-lateral lead ( = lead I).
- BOTTOM Line: The above clearly represents a series of "soft" ECG signs that to me suggested a less "anatomic" distribution of ST-T wave changes than I would expect with acute OMI. ECG findings somewhat atypical for acute OMI in a teenager clearly increase suspicion for acute myocarditis.
=============================
Acute MI in Children:
- I list in Figure-2 — potential causes of acute MI to consider in the pediatric age group (Suryawanshi et al — Ann Pediatr Cardiol 4(1):81-83, 2011).
- I've listed potential causes of acute pericarditis in My Comment at the bottom of the page in the June 11, 2022 post in Dr. Smith's ECG Blog.
- Potential causes of acute myocarditis (or acute perimyocarditis) — are similar to those causing pure acute pericarditis.
-USE.png) |
| Figure-1: Potential Causes of acute MI in Children (Adapted from Suryawanshi et al — Ann Pediatr Cardiol 4(1):81-83, 2011). |


-USE.png)
No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.