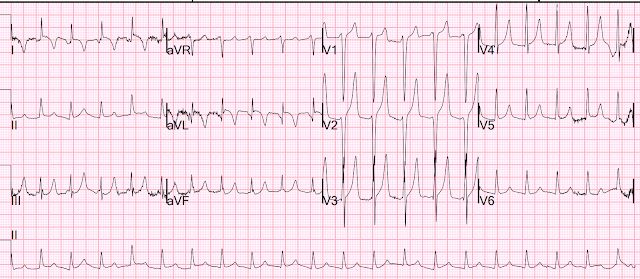
I was reading EKGs on the system and came across this one:
What do you think?
This is diagnostic of hyperkalemia. HyperK can result in all sorts of pseudoSTEMI or pseudoOMI patterns, including ST elevation, ST depression, and large T-waves.
These T-waves are tall but have a narrow base and a corresponding flat ST segment (see lead V4). Also, there are no definite P-waves and this is another result of hyperkalemia. In fact, sometimes the sinus node is working and acting as a pacemaker but no P waves are visible!! This is called sino-ventricular rhythm. See these 3 other posts of sinoventricular rhythm
The K came back at 6.2 mEq/L.
The patient was treated.
He ruled out for MI by troponins.
No followup EKG was recorded!!
See many examples of Pseudo STEMI due to hyperkalemia at these two posts:
Acute respiratory distress: Correct interpretation of the initial and serial ECG findings, with aggressive management, might have saved his life.
===================================
MY Comment by KEN GRAUER, MD (2/27/2023):
===================================
One of the most common "ECG Emergencies" entails prompt recognition of Hyperkalemia — with our goals being: i) Avoidance of misdiagnosis (ie, mistaking tall, peaked T waves for deWinter T waves — as seemed to occur in today's case); and, ii) Prompt treatment of this potentially life-threatening condition (ie, with calcium) — which should often be given prior to lab confirmation of hyperkalemia, because cautious administration of IV calcium is safe — and not-to-promptly treat the patient risks losing the patient.
We've presented numerous examples of hyperkalemia on Dr. Smith's ECG Blog. Today's case presents a few more of the "Many Faces" of Hyperkalemia that are important for us to appreciate. I'd add the following to Dr. Smith's discussion:
- As always — I favor beginning my assessment with a Systematic Approach. Descriptive analysis of the ECG in today's case reveals a regular, narrow tachycardia at ~130/minute, without clear sign of sinus P waves.
- QRS amplitude appears increased in several chest leads (ie, very deep S waves in leads V1,V2 — large isoelectric complex in V3).
- There appears to be a Q wave in lead aVL — though limb lead artifact makes this difficult to assess.
- As per Dr. Smith — T waves in multiple leads are tall, peaked, and manifest a narrow base. This is especially true in leads V2,V3 — in which T wave amplitude exceeds 15 mm! Of note — these T waves are symmetric, with similarly angled ascending and descending limbs of the T wave.
- BOTTOM LINE: As per Dr. Smith — this ECG is diagnostic of Hyperkalemia until you prove otherwise.
QUESTIONS:
- What is the rhythm?
- Given how tall the T waves are and the lack of P waves — Why isn't the QRS wide?
- Why isn't the serum K+ higher than 6.2 mEq/L?
- Why is there T wave inversion in leads I and aVL?
- Finally — Could anything else be going on with this patient?
===================================
WHAT is the Rhythm in Today's Case?
Dr. Smith suggests that the rhythm in today's case is sinoventricular rhythm — because it is common with hyperkalemia for sinus node activity to continue (at least for a while) despite the disappearance of P waves on ECG.
- In today's case — I fully acknowledge that I do not know for certain what the rhythm is. The QRS is narrow — and no P waves are seen. But the rate is ~130/minute — which is a bit fast for sinus tachycardia. So IF this is sinus tachycardia with a sinoventricular rhythm — then we have to explain WHY the rate is this fast.
- Alternatively — the rhythm could be junctional tachycardia ...
- Finally — it almost looks like there are 2 equally spaced upright deflections in lead aVR, which if true might indicate 2:1 AFlutter.
- BOTTOM Line: Practically speaking — it does not matter what the rhythm in today's case is — because IF this patient would be promptly treated with Calcium — whatever this rhythm was would most probably rapidly resolve.
As a reminder of why determination of the cardiac rhythm can be so challenging when there is significant hyperkalemia — I've reproduced Figure-1 from My Comment in the January 16, 2022 post in Dr. Smith's ECG Blog.
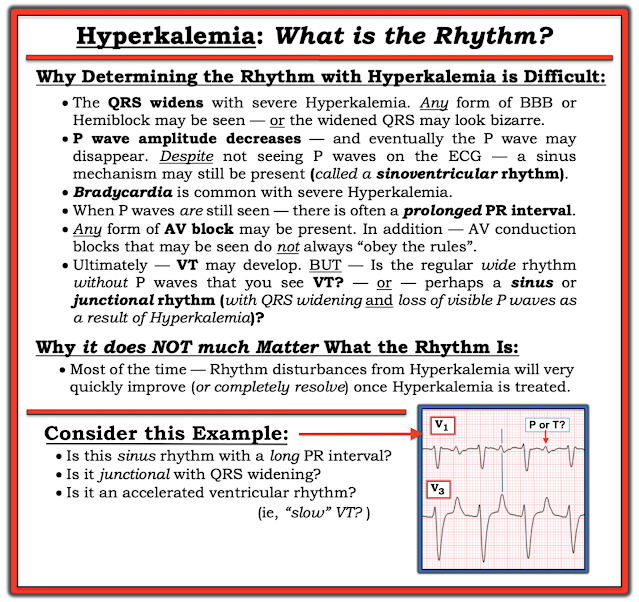 |
| Figure-1: Reasons for the difficulty determining the rhythm with severe hyperkalemia. |
WHY Isn't the QRS Wide?
I think it helpful to appreciate the "textbook" sequence of ECG findings seen with progressive degrees of hyperkalemia. While fully acknowledging that "not all patients read the textbook" — I have found awareness of the ECG generalizations in Figure-2 to be extremely helpful.
- TO EMPHASIZE — Not all patients follow the sequence of ECG changes shown below in Figure-2. For example — some patients may develop everything except QRS widening. Others may not show T wave peaking — or may only show this finding as a later change. And despite marked hyperkalemia — some patients may not show any ECG changes at all.
- The above said — Over the years, I have found Figure-2 to be helpful as a guide that does hold true in a significant percentage of patients.
- P.S.: There are times when even before the serum K+ value returns from the lab — you know from the ECG that there is severe (life-threatening) hyperkalemia. For example — marked bradycardia with unusual forms of advanced AV block — or marked bradycardia without evident P waves — or marked QRS widening with "shapeless" morphology — are all ECG indication of the need for immediate IV calcium until improvement of these ECG patterns.
 |
| Figure-2: The “textbook” sequence of ECG findings with hyperkalemia. (I've reproduced this figure from My Comment in the January 6, 2020 post of Dr. Smith's ECG Blog). |
Why Isn't the Serum K+ Higher than 6.2 mEq/L?
Despite the lack of atrial activity and the extremely tall T waves in multiple leads — the serum K+ value of 6.2 mEq/L is not overly high. Judging by the ECG in today's case — I would have anticipated a higher value. Several reasons may explain this lower-than-expected serum K+ value:
- As emphasized above — the "textbook" sequence shown above in Figure-2 is not perfectly followed by all patients.
- Certain conditions (ie, DKA) may be associated with rapid intra-extracellular K+ shifts — such that serum values can change quickly.
- There is often missing documentation as to when which ECG was recorded at the time of which blood draw (and whether any treatment had yet been initiated). So the 6.2 mEq/L K+ value may (or may not) closely correlate to the timing of today's ECG.
Why is there T Wave Inversion in Leads I and aVL?
Much attention focuses on the appearance of tall, peaked and pointed T waves in association with hyperkalemia. Not commonly appreciated — is that sometimes, you may see deep, symmetric and pointed T wave inversion in a number of leads. This is usually not ischemic — but rather another ECG manifestation of hyperkalemia.
- Aren't those deep, symmetric T wave inversions in leads I and aVL the virtual "mirror-image opposite" of the tall, pointed upright T waves in leads III and aVF?
Could Anything Else Be Going On?
We are told that the patient in today's case was ruled out for MI — but that no follow-up ECG was recorded. In my opinion — Not recording a follow-up ECG after treatment of hyperkalemia was a mistake!
- The ECG of a patient with hyperkalemia shows the net effect of what underlying ST-T waves looked like before development of the tall, peaked T waves of hyperkalemia. Only after correcting hyperkalemia and repeating the ECG — will you be able to determine whether ischemic ST-T wave changes exist.
- This point is especially relevant in today's case — because the T waves in many leads are especially tall (and there is also deep T wave inversion in leads I and aVL). TO EMPHASIZE — Although I suspect that all ST-T wave abnormalities will normalize with correction of the hyperkalemia in today's case — we do not know this for certain without repeating the ECG.
- The other reason why the ECG in today's case should have been repeated after correction of hyperkalemia — is that the only cardiac rhythm documented in this case is an SVT at ~130/minute without sinus P waves. We do not know for certain what the rhythm was? And, there is no documentation that the tachycardia has resolved.

No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.