Case submitted by Matt Tanzi MD, written by Pendell Meyers
A man in his early 50s presented with substernal chest pain and that started 1 hour prior to arrival. There was some radiation to the left jaw and diaphoresis. He had ongoing pain on arrival.
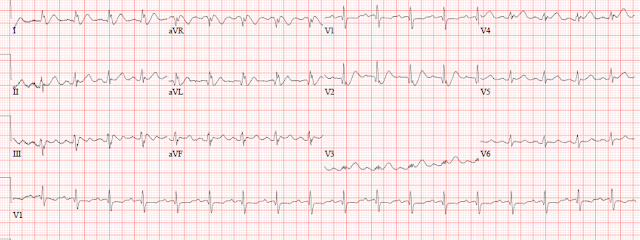
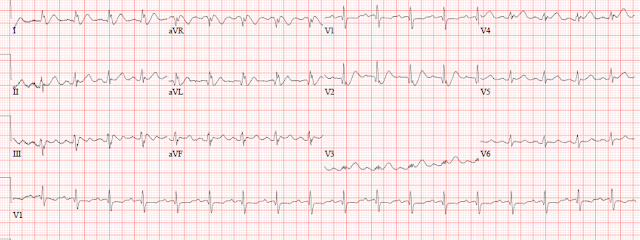
Initial triage ECG:
I sent this to Dr. Smith who immediately replied that it is diagnostic of OMI, but difficult to tell whether it is 1) anterolateral with de Winter morphology, or instead 2) A combination of Aslanger's pattern (inferior OMI with single lead STE in III and reciprocal STD in I, aVL, plus widespread STD of subendocardial ischemia) with posterior (V2 STD) and RV extension (V1 STE). In other words, does V2 indicate ST depression of posterior OMI? or is the ST depression and hyperacute T wave indicative of de Winter hyperacute OMI morphology of the anterior wall? It is difficult to tell, but either way: OMI needing reperfusion.
The ECG shows sinus tachycardia, grossly normal QRS complex, ST depression from V2-V6, and in I and aVL. There are possibly hyperacute T waves in V2 (maybe also V3 and V4), constituting de Winter morphology (hyperacute T wave taking off from depressed ST segment). V1 has a tiny amount of STE and a hyperacute T wave also. The ECG overall is diagnostic of OMI.
The cath lab was activated. He received aspirin and heparin bolus. The cardiologist immediately evaluated the patient and stated that the ECG did not meet STEMI criteria, so the cath lab was cancelled. The cardiologist stated that they should try nitroglycerin and see if that controls the pain.
He was given sublingual nitro and then a continuous drip.
ED2 Post nitro:
 |
| Mostly similar, but ST segments in V3 and V4 have risen. Still de Winter morphology in V2, I, and aVL. |
|
At this time, POCUS was performed by the ED team and is shown below:
I believe the POCUS clips above show a clear anterior wall motion abnormality.
The patient had ongoing chest pain. The ultrasound was reviewed with the cardiologist and together they reactivated the cath lab, about 25 minutes after the initial cancellation.
If you had waited for the initial (conventional prior generation) Troponin T, it was undetectable (less than 0.01 ng/mL).
Angiogram results:
Prox LAD 99%, thrombectomy (no TIMI flow listed)
"Distal nitroprusside administration and distal LAD thrombectomy performed with improvement in no reflow."
"Integrellin double bolus given in lab. Continue Integrelin for 18 hours."
Post cath ECG:
 |
What do you think? What has changed?
|
|
Now there is RBBB (the right bundle is supplied by the LAD in all cases I am aware of), with persistent concordant STE in precordial leads, as well as Q-waves in V1 and V2. In the situation of LAD OMI, this ECG does not yet show significant signs of reperfusion, and may instead be concerning for No Reflow phenomenon, meaning lack of downstream perfusion despite epicardial intervention.
Formal echo next day:
Severely reduced global LF systolic function, EF 25%
WMA: mid anterior, mid anterolateral, mid inferior, mid anterior septum, inferior septum, entire apex, all severely hypokinetic
No evidence of clot with usage of echo enhancing agent. Swirling of contrast in LV apex consistent with low flow state
Normal RV systolic function
Peak Troponin T = 4.94 ng/mL (large MI, similar to the average STEMI+OMI in our data of 265 OMIs, using the same assay, which had mean and median peak troponin T of 5.50 and 3.78 ng/mL)
Discharge ECG:
 |
| Persistent RBBB. The Q wave in V1-2 has widened, concerning for LV aneurysm morphology in RBBB. There is conspicuous lack of reperfusion T wave inversions in anterolateral areas, which would usually be present if there had been meaningful reperfusion. This ECG further supports No Reflow and long term poor outcome. |
|
Learning Points:
When the OMI is most hyperacute, when there is maximal tissue to be salvaged by emergent reperfusion therapy, the troponin is lowest and there is very often insufficient STE to meet STEMI criteria. We have shown that, even in OMIs that DO meet STEMI criteria, expert ECG interpretation can identify OMI hours sooner than STEMI criteria. Would you like your EM physician and cardiologist to be ECG experts? or just use STEMI criteria?
When the ECG is not diagnostic to a provider, immediate bedside echo can help to diagnose OMI.
The LAD supplies the RBBB and LAFB. New RBBB/LAFB in OMI is a sign of extremely dangerous LAD OMI.
No Reflow phenomenon indicates inadequate downstream reperfusion and is diagnosable by ECG.
===================================
MY Comment, by KEN GRAUER, MD (9/22/2022):
===================================
I liked this case — because it presents yet one more variation in the de Winter T Wave Pattern that we all need to recognize.
- For clarity — I have reproduced and show together in Figure-1 — the first 2 tracings in today's case.
Dr. Meyers showed Dr. Smith and myself the 1st ECG in today's case, initially without the benefit of any history. As noted above — Dr. Smith was immediately suspicious of, "de Winter, LAD OMI".
I focus my comment on my slightly different response. I replied as follows for my interpretation of ECG #1:
- "Sinus tachycardia — some potentially significant Q waves (in leads aVL, V1,V2) — and LOTS of ST depression, which interestingly is most marked in lead V2 (!), as well as in high-lateral leads I and aVL. In addition — there is ST elevation in “opposing” leads (ie, especially in lead aVR — but also in leads III and V1)."
- My Impression of ECG #1 was: "Diffuse subendocardial ischemia in a patient with multi-vessel disease (and probably some prior events). IF associated with a history of new chest pain — then this patient should clearly undergo prompt cath to define the anatomy."
The reason why I did not promptly recognize de Winter T Waves (as Dr. Smith immediately did) — was because I didn't see very tall T waves arising from the marked J-point ST depression.
- The "Take Home" point for me regarding today's case — was that the simple reason I didn't see the very tall anterior T waves usually associated with de Winter T Waves — is that we were seeing this extensive anterior infarction at a very early stage in the process before the T waves had a chance to enlarge.
- I believe the process in today's patient did begin with diffuse subendocardial ischemia (supported by the diffuse severe hypokinesis on formal Echo done the following day).
- Then followed initial marked J-point ST depression (in leads I, aVL and V2 — as seen in ECG #1 of Figure-1) — with development of terminal T wave positivity in these 3 leads.
- And as we look back on ECG #1 (after seeing the subsequent serial ECGs that evolved) — those Q waves I pointed out in ECG #1 were in fact early indicators of the infarction to come.
- The follow-up ECG (ECG #2 — done a short while later) — then showed progression of extensive evolving infarction. Specifically — the amount of J-point ST depression in leads I, aVL and V2 is much less in ECG #2 (with reduction in the amount of ST depression in other chest leads) — and T waves in multiple leads (ie, leads I, II, aVL; V2,V3,V4) are becoming larger and "fatter"-at-their-peak (ie, more hyperacute).
-USE.png) |
| Figure-1: The first 2 ECGs in today's case. |
Additional Learning Points from Today's Case:
We continue to frequently review the gamut of de Winter T Wave "variants" in Dr. Smith's ECG Blog (See the May 2, 2019 post — among many others). - I discussed in detail in My Comment at the bottom of the page in the July 11, 2022 post — how common it is to see "variations on the theme" of de Winter T Waves. In the interest of brevity — I'll simply reproduce in Figure-2, my adaptation from the original manuscript by de Winter et al, published in this 2008 NEJM citation — which shows you 8 selected ECG presentations from his series of patients.
- I've seen scores of other variations of de Winter T Waves. I have added to "My Mental List" — the additional ECG variation seen in ECG #1 from today's case, in which we catch a very early glimpse of de Winter T waves evolving from initial diffuse subendocardial ischemia.
- P.S.: Clinically — the fact that I did not recognize de Winter T waves as soon as Dr. Smith did in today's case does not matter — because regardless of what you call the picture of ECG #1 in Figure-1 — in a patient with new-onset chest pain — prompt cardiac cath is clearly indicated. Unfortunately that was not done in today's case.
 |
| Figure-2: The de Winter T Wave Pattern, as first described by Robbert J. de Winter et al in N Engl J Med 359:2071-2073, 2008. ECGs for the 8 patients shown here were obtained between 26 and 141 minutes after the onset of symptoms. (See text). |





-USE.png)
No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.