A 60-something female presented with episodes of chest pain for the previous 2 days that lasted 20 to 30 minutes each. On the day of presentation, her episode lasted much longer and she came to the emergency department. In the ambulance, she was given nitro and her pain was relieved. On arrival to the emergency department she was pain free.
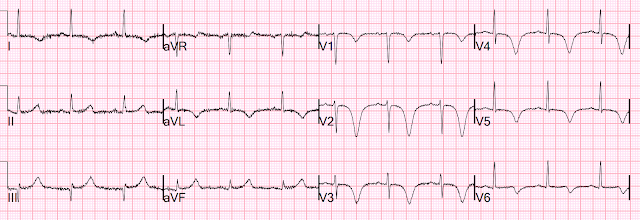
This is classic Wellens' pattern B morphology, and fits with the entire presentation.
So it is Wellens' syndrome. The ECG is so classic that when I saw the ECG on the system, I knew it was the full syndrome and wrote that "this patient would be pain free at this moment." Then I confirmed that when I went to the chart.
See important description of Wellens' syndrome below.
The providers who saw the patient were concerned about inferior OMI due to the subtle STE in inferior leads, and STD in aVL.
How do we KNOW it is not active inferior OMI?
1. The patient is completely pain free and 2. Such inferior STE, and even apparent hyperacute T-waves, are commonly reciprocal to anterior and high lateral reperfusion.
Here is a similar case:
How do you explain these inferior hyperacute T-waves?
1 hour later:
Further evolution (deepening) of symmetric T-wave inversion in precordial leads
Angiogram:
Acute MI Non ST Elevation Myocardial Infarction .
Culprit is 90% stenosis in the proximal LAD .
After PCI:
2 days later
Wellens' syndrome
Wellens' syndrome is a syndrome of Transient OMI (including transient STEMI) of the LAD, in which the ECG was not recorded at the time of the anginal pain, but only after sponaneous resolution of the pain, at which time the ECG shows reperfusion T-waves in the LAD distribution. Pattern A = terminal T-wave inversion (biphasic); Pattern B shows deep symmetric T-wave inversion. Wellens' syndrome also requires preservation of R-waves.
Thus, in Wellens' syndrome, the patient is:
1) Pain free after an episode of angina,
2) Has a typical T-wave inversion morphology (not all T-wave inversion is Wellens!!),
3) Will have preserved R-waves
4) Will have evolution of the T-wave inversion,
5) Will always have some rise and fall of troponin,
6) Will have an OPEN artery OR good collateral circulation (the myocardium is perfused)
7) At high risk of re-occlusion (with pseudonormalization of T-waves if it occurs)
Such T-wave inversion also occurs in all the other coronary distributions.
See these posts for a variety of Wellens and mimics:
===================================
MY Comment, by KEN GRAUER, MD (8/12/2022):
===================================
An appreciation of Wellens' Syndrome is a must in emergency care. The "beauty" of this clinical entity is 3-Fold: i) Awareness of what to look for in the History and in the ECG allows diagnosis within seconds (as per Dr. Smith's instant analysis in today's case); ii) Recognition of Wellens' Syndrome tells you the anatomy (ie, accurate prediction of a high-grade proximal LAD stenosis); and, iii) Recognition of Wellens' Syndrome prompts the need for timely cath and life-saving treatment.
- In addition to today's case — we've posted numerous examples of Wellens' Syndrome on Dr. Smith's ECG Blog (See the June 28, 2018 post — and the December 14, 2018 post — to name just 2 instances).
- Unfortunately, despite the above expert commentary by Dr. Smith in today's case — Wellens' Syndrome remains a misunderstood diagnosis by all too many healthy care providers.
The History of Wellens' Syndrome:
It's hard to believe that the original manuscript describing Wellens' Syndrome was published 40 years ago! As I contemplated today's case — I thought it would be insightful to go back to this original manuscript (de Zwaan, Bär & Wellens: Am Heart J 103: 7030-736, 1982):
- The authors (de Zwaan, Bär & Wellens) — studied 145 consecutive patients (mean age 58 years) admitted for chest pain, thought to be having an impending acute infarction (Patients with LBBB, RBBB, LVH or RVH were excluded). Of this group — 26/145 patients either had or developed within 24 hours after admission, a pattern of abnormal ST-T waves in the anterior chest leads without change in the QRS complex.
- I've reproduced (and adapted) in Figure-1 — prototypes of the 2 ECG Patterns seen in these 26 patients. Of note — all 26 patients manifested characteristic ST-T wave changes in leads V2 and V3.
- Most patients also showed characteristic changes in lead V4.
- Most patients showed some (but less) ST-T wave change in lead V1.
- In occasional patients — abnormal ST-T waves were also seen as lateral as in leads V5 and/or V6.
- Half of the 26 patients manifested characteristic ST-T wave changes at the time of admission. The remaining 13/26 patients developed these changes within 24 hours after admission.
- Serum markers for infarction (ie, CPK, SGOT, SLDH) were either normal or no more than minimally elevated.
ECG Patterns of Wellens' Syndrome:
The 2 ECG Patterns observed in the 26 patients with characteristic ST-T wave changes are shown in Figure-1:
- Pattern A — was much less common in the study group (ie, seen in 4/26 patients). It featured an isoelectric or minimally elevated ST segment takeoff with straight or a coved (ie, "frowny"-configuration) ST segment, followed by a steep T wave descent from its peak until finishing with symmetric terminal T wave inversion.
- Pattern B — was far more common (ie, seen in 22/26 patients). It featured a coved ST segment, essentially without ST elevation — finishing with symmetric T wave inversion, that was often surprisingly deep.
-USE%20copy.png) |
| Figure-1: The 2 ECG Patterns of Wellens' Syndrome — as reported in the original 1982 article (Figure adapted from de Zwaan, Bär & Wellens: Am Heart J 103:730-736, 1982). |
ST-T Wave Evolution of Wellens' Syndrome:
I've reproduced (and adapted) in Figure-2 — representative sequential ECGs obtained from one of the patients in the original 1982 manuscript.
- The patient whose ECGs are shown in Figure-2 — is a 45-year old man who presented with ongoing chest pain for several weeks prior to admission. His initial ECG is shown in Panel A — and was unremarkable, with normal R wave progression. Serum markers were negative for infarction. Medical therapy with a ß-blocker and nitrates relieved all symptoms.
- Panel B — was recorded 23 hours after admission when the patient was completely asymptomatic. This 2nd ECG shows characteristic ST-T wave changes similar to those shown for Pattern B in Figure-1 (ie, deep, symmetric T wave inversion in multiple chest leads — with steep T wave descent that is especially marked in lead V3).
- Not shown in Figure-2 are subsequent ECGs obtained over the next 3 days — that showed a return to the "normal" appearance of this patient's initial ECG (that was shown in Panel A of Figure-2). During this time — this patient remained asymptomatic and was gradually increasing his activity level.
- Panel C — was recorded ~5 days later, because the patient had a new attack of severe chest pain. As can be seen — there is loss of anterior forces (deep QS in lead V3) with marked anterior ST elevation consistent with an extensive STEMI. Unfortunately — this patient died within 12 hours of obtaining this tracing from cardiogenic shock. Autopsy revealed an extensive anteroseptal MI with complete coronary occlusion from fresh clot at the bifurcation between the LMain and proximal LAD.
-USE%20copy.png) |
| Figure-2: Representative sequential ECGs from one of the patients in the original 1982 article. Panel A: The initial ECG on admission to the hospital; Panel B: The repeat ECG done 23 hours after A. The patient had no chest pain over these 23 hours. NOTE: 3 days after B — the ECG appearance of this patient closely resembled that seen in A ( = the initial tracing). Panel C: 5 days later — the patient returned with a new attack of severe chest pain. As seen from this tracing (C) — this patient evolved a large anterior STEMI. He died within hours from cardiogenic shock (Figure adapted from de Zwaan, Bär & Wellens: Am Heart J 103:730-736, 1982 — See text). |
Relevant Findings from the 1982 Article:
The ECG pattern known as Wellens' Syndrome was described 40 years ago. Clinical findings derived from the original 1982 manuscript by de Zwaan, Bär & Wellens remain relevant today.
- One of the 2 ECG Patterns shown in Figure-1, in which there are characteristic anterior chest lead ST-T wave abnormalities — was seen in 18% of 145 patients admitted to the hospital for new or worsening cardiac chest pain.
- Variations in the appearance of these 2 ECG patterns may be seen among these patients admitted for chest pain. Serial ECGs do not show a change in QRS morphology (ie, no Q waves or QS complexes developed). Serum markers for infarction remain normal, or are no more than minimally elevated.
- Among the subgroup of these patients in this 1982 manuscript who did not undergo bypass surgery — 75% (12/16 patients) developed an extensive anterior STEMI from proximal LAD occlusion within 1-2 weeks after becoming pain-free.
LESSONS to Be Learned:
At the time the 1982 manuscript was written — the authors were uncertain about the mechanism responsible for the 2 ECG patterns of Wellens' Syndrome.
- We now know the mechanism. A high percentage of patients seen in the ED for new cardiac chest pain that then resolves — with development shortly thereafter of some form of the ECG patterns shown in Figure-1 — had recent coronary occlusion of the proximal LAD — that then spontaneously reopened.
- The reason Q waves do not develop on ECG and serum markers for infarction are normal (or at most, no more than minimally elevated) — is that the period of coronary occlusion is very brief. Myocardial injury is minimal (if there is any injury at all).
- What spontaneously occludes — and then spontaneously reopens — may continue to reocclude, and then reopen — until eventually a final disposition is reached (ie, with the "culprit" vessel staying either open or closed).
- As per the above discussion by Dr. Smith — We can know whether the "culprit" artery is either open or closed by correlating serial ECGs with the patient's history of chest pain. For example, in today's case — the finding of deep, symmetric T wave inversion in virtually all chest leads in association with resolution of the chest pain immediately told Dr. Smith that the LAD had spontaneously reopened.
- The importance of recognizing Wellens' Syndrome — is that it tells us that timely cardiac cath will be essential IF we hope to prevent reclosure. In the de Zwaan, Bär & Wellens study — 75% of these pain-free patients with Wellens' ST-T wave changes went on to develop a large anterior STEMI within the ensuing 1-2 weeks if they were not treated.
- Thus, the goal of recognizing Wellens' Syndrome — is to intervene before significant myocardial damage occurs (ie, diagnostic criteria for this Syndrome require that anterior Q waves or QS complexes have not developed — and serum markers for infarction are no more than minimally elevated).
- It is not "Wellens' Syndrome" — IF the patient is having chest pain at the time the ECG patterns in Figure-1 are seen. Active chest pain suggests that the "culprit" artery has reoccluded.
- Exclusions from the 1982 study were patients with LBBB, RBBB, LVH or RVH. While acute proximal LAD occlusion can of course occur in patients with conduction defects or chamber enlargement — Recognition of the patterns for Wellens' Syndrome is far more challenging when any of these ECG findings are present.
- Finally — a word about the ECG Patterns of Wellens' Syndrome shown in Figure-1 is in order. Pattern A — is far less common, but more specific for Wellens' Syndrome IF associated with the "right" history (ie, prior chest pain — that has now resolved at the time ST-T wave abnormalities appear).
- Unlike the example in Figure-1 — Pattern B may be limited to symmetric T wave inversion without the finding of steep T wave descent into terminal negativity in any lead. This is the pattern seen in today's case — which given the history, was immediately diagnosed as Wellens' Syndrome by Dr. Smith.
In Conclusion — the 145 pts studied by de Zwaan, Bär & Wellens in 1982 continue to provide clinical insight into the nature of Wellens' Syndrome some 40 years after this manuscript was written.
- P.S.: And sometimes — there may be a similar evolution of ECG findings indicative of acute occlusion and spontaneous reperfusion (corresponding to changes in chest pain severity) in not only anterior leads — but also in the inferior leads. As per Dr. Smith in today's case — this is not active acute inferior OMI — but rather a "reciprocal part" of the Wellens' Syndrome evolution.





No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.