This was sent by one of our faculty, Steven Souchtchenko, who trained under me and works at another hospital most of the time, and with us at Hennepin some of the time.
Case:
53yoF with stuttering CP for 2 days, suddenly acutely worse tonight, now 10/10 pressing radiating to L arm.
Steven wrote:
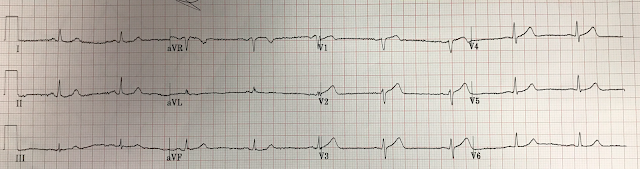
"I called it "OMI" based on hyperacute T-waves." (Dr. Souchtchenko understands that a hyperacute T-wave is not at all defined by its height, nor even by its size and bulk (though these are "bulky," but by its size in proportion to the QRS).
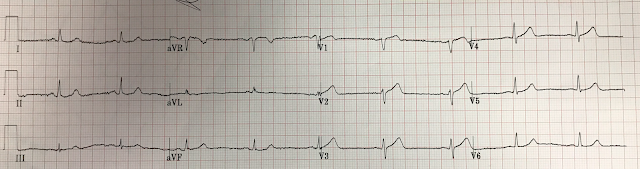
"Cardiology didn’t believe me. I recorded a right sided ECG 16 minutes later." Here is the right sided ECG he recorded:
Look at the first ECG again, and use the 4 variable formula to distinguish normal ST Elevation in V2-V4 from STE in V2-V4 that is due to LAD occlusion:
Again, for many examples of use of the formula, go to this blog post:
12 Example Cases of Use of 3- and 4-variable formulas, plus Simplified Formula, to differentiate normal STE from subtle LAD occlusion
Case continued
The initial troponin I returned at 0.146 ng/mL
The patient was taken for an angiogram:
95% LAD stenosis with TIMI-3 flow. It was stented.
The post cath (but not necessarily peak), troponin I was 0.846 ng/mL. This is not very high for OMI, but can be seen if the artery is only briefly occluded (whether due to very fast intervention or spontaneous reperfusion).
In our studies (see this one), we define OMI as:
1) TIMI 0-2 flow, or
2) Culprit + TIMI-3 flow + peak troponin of at least 10.0 ng/mL for troponin I, 1.0 ng/mL for trop T, or 1000 ng/L for hs trop T.
So this case would qualify as a "false positive" using these research methods. But it clearly is not a false positive!! In other words, these research methods result in false false positives. This is a necessary limitation of the research originating from the fact that we don't record the ECG at the same time as the angiogram, and thrombosis is dynamic, with thrombus alternately spontaneously lysing and propagating.
Nevertheless, we must report them as false positives in our papers, even though they are actually true positives for OMI (false false = true).
The timing of ECG recording:
Had this ECG been recorded at some time point when there was TIMI-3 flow for an extended period, the OMI would not have been apparent. The patient would have had an unrecorded transient STEMI and perhaps re-occluded in the middle of the night. This is why it is so important to try to record an ECG during pain, not only AFTER pain or during gradual resolution of pain.
- In addition to satisfying Dr. Smith's 4-variable formula that supports LAD occlusion — I thought there were ST-T wave abnormalities consistent with at-the-least possible (if not probable) acute LAD OMI in at least 9/12 leads (Figure-1).
-USE.png) |
| Figure-1: The initial ECG in today's case. (To improve visualization — I've digitized the original ECG using PMcardio). |
- When faced with subtle-but-definitely-present ECG findings (as occurred in today's case) — I favor focusing my assessment on those leads that I know are clearly abnormal. In Figure-1 — I've enclosed the 2 leads with the most obviously abnormal ST-T waves within RED-YELLOW rectangles. In a patient with new worrisome chest pain — the T wave in lead V2 is clearly disproportionate compared to the QRS complex in this lead (ie, the T wave in V2 towers over its respective R wave — with a T wave that is fatter-at-its-peak and wider-at-its-base than it should be).
- NOTE: Although the T wave in lead V2 might not seem all that tall — what counts is proportion. The QRS complex in V2 is quite small — and relative to the small size of this QRS — there should be no doubt that the T wave in this lead is clearly too big.
- Although slightly less disproportionate — the T wave in lead V3 is still "too tall" (it equals R wave amplitude in this lead) — with a wider-than-expected base.
- By the principle "neighboring leads" (ie, knowing that the ST-T waves in leads V2,V3 are hyperacute until proven otherwise) — I thought the T wave in lead V4 was probably also "hypervoluminous". By itself — lead V1 might not be taken as necessarily "abnormal" — but most of the time, a straight takeoff with a 1.5 mm tall positive T wave will not be seen in this lead (so given its proximity to lead V2 that is definitely abnormal — I thought it likely that the ST-T wave in lead V1 was probably also hyperacute).
- Changes in the limb leads were even more subtle — but nevertheless clearly present. While fully acknowledging that the ST segment straightening (highlighted in Figure-1 by RED lines) by itself would be non-specific — in the context of a patient with a history of very worrisome chest pain + at least 2 (if not 4) chest leads showing hyperacute T waves — I interpreted these limb lead abnormalities as adding support to suspicion of acute OMI until proven otherwise.
- For clarity — I have enlarged these 2 leads from ECG #2 ( = the right-sided ECG) — so that we can assess the effect of the repeat ECG done 16 minutes later on leads V1 and V2 (See Figure-2).
- Always considering the clinical context (which in today's case was the very worrisome history for acute cardiac chest pain). Faced with this history — I lower my threshold for calling subtle ECG findings abnormal until proven otherwise.
- Looking for ECG findings in those 1 or 2 leads in which you know that ST-T wave appearance is not-as-it-should-be.
- Applying the concept of "neighboring leads" — in which more subtle ST-T wave findings are probably also abnormal, if seen in leads in close proximity to leads that you know are abnormal.
- Looking to see how many of the 12 leads show ST-T wave abnormalities (even if some of these abnormalities are subtle). The more leads that are abnormal in a patient with new chest pain — the greater the likelihood that an acute process is ongoing.





-USE.png)
No comments:
Post a Comment
DEAR READER: I have loved receiving your comments, but I am no longer able to moderate them. Since the vast majority are SPAM, I need to moderate them all. Therefore, comments will rarely be published any more. So Sorry.