===================================
MY Comment by KEN GRAUER, MD (7/14/2020):
===================================
This middle-aged man with hypertension and hyperlipidemia presented to the ED with 2 hours of new-onset chest pain — and the ECG shown in Figure-1. The patient was hemodynamically stable. No prior tracing was available for comparison.
- HOW would you interpret the ECG shown in Figure-1?
- Immediate cath lab activation was not an option in this hospital. Should acute thrombolysis be used?
 |
| Figure-1: The initial ECG in the ED (See text). |
My THOUGHTS on ECG #1: I’ve labeled KEY findings in Figure-2. The rhythm in ECG #1 is sinus tachycardia at ~110-115/minute. The PR interval is normal — but the QRS complex is wide. The QTc appears prolonged — but this is difficult to assess given the rapid rate.
- QRS morphology is consistent with complete RBBB (ie, widened QRS; qR pattern with predominant positivity in lead V1 — wide terminal S waves in lateral leads I and V6).
- The initial Q wave, with qR pattern (instead of an rsR’ complex) in lead V1 is important to note (within the RED circle in lead V1 of Figure-2). This finding may indicate septal infarction of uncertain age.
- A large and wider-than-it-should-be Q wave is seen in lead III (ie, this Q in III is “large” considering the modest amplitude of the R wave in this lead). A tiny q wave is also seen in lead aVF — but no Q wave is seen in lead II. The significance of these inferior Q waves is uncertain.
- There is no chamber enlargement.
- The most remarkable finding is diffuse ST depression in no less than 9 of 12 leads. The indistinct boundary between the end of the S wave (of the QRS complex) and the J-point that marks the beginning of the ST segment, makes it challenging to quantitate the precise amount of ST depression in some leads. For clarity — I’ve drawn short horizontal RED lines at the point I believe indicates the amount of ST depression — which is considerable given the modest R wave amplitude in most leads.
- There is ST elevation in lead aVR (horizontal BLUE line indicating the amount).
Clinical IMPRESSION: Given the history of new-onset chest pain — the findings in ECG #1 are extremely concerning:
- There is sinus tachycardia at 110-115/minute.
- There is complete RBBB — with a Q wave in lead V1 consistent with septal infarction of uncertain age. Without any prior tracing for comparison — it’s impossible to know if the RBBB is new or old.
- The Q waves in leads III and aVF, together with a difficult-to-interpret ST segment in lead III (that possibly was recently elevated) could be consistent with inferior infarction of uncertain age. I suspect this is not new.
- The marked, diffuse ST depression, with ST elevation in lead aVR is consistent with diffuse subendocardial ischemia. Given the clinical scenario — the most likely cause of this finding is severe coronary disease (ie, LMain, proximal LAD, or multi-vessel disease) — but not acute OMI.
PEARL: We expect to see a negative ST-T wave in anterior leads with RBBB. That said — We do not expect to see the following with “typical” RBBB:
- Coving of the ST segment in lead V1 (as per the curved BLUE line in this lead).
- A ledge-like (flat) shape for the ST depression that we see in leads V2 and V3.
- An increasing amount of ST depression as we move across the chest leads (ie, ST depression in ECG #1 is maximal in lead V3, and remains significant through to lead V6 — instead of being maximal in leads V1, V2 as should be seen with typical RBBB).
- Typical RBBB generally produces an upright T wave without ST depression in lateral leads. It does not produce the ST depression we see here in leads I, aVL; V4, V5 and V6.
We’ve discussed the entity of diffuse subendocardial ischemia on many occasions in Dr. Smith’s ECG Blog (For 1 example — SEE discussion by Dr. Smith + My Comment at the bottom of the page in the May 13, 2020 post).
- An important Learning Point from today’s case is recognizing subendocardial ischemia despite the presence of complete RBBB.
- For discussion on management of this case — SEE comments below by Dr. Smith.
================
- NOTE: My sincere THANKS to Dr. Eduardo Lapa (from Brazil) for sharing the tracing and this case with us!
================
COMMENT by Dr. SMITH:
This ECG manifests diffuse subendocardial ischemia. But ischemia can be caused by ACS or by non-ACS etiologies (due to supply demand mismatch). Only the clinical context can illuminate this. The clinical scenario (onset of chest pain at rest) strongly suggests ACS. But the clinician must be certain it is not sepsis, GI bleed, respiratory failure, pulmonary embolism, decompensated aortic stenosis, or other etiologies, before concluding that it is indeed ACS.
This is not only severe coronary artery disease (CAD): the ECG and symptoms are both ACUTE, with active ischemia. Active ischemia is not a chronic condition; CAD is a chronic condition. So if this is indeed this is ACS, then there is severe CAD with plaque rupture and thrombus. People can have severe coronary disease, but if they have sudden chest pain and active ischemia, they have acute coronary syndrome. However, this is indeed not an OMI, because there is flow in the artery, but there is most likely thrombus with insufficient flow.
See these posts:
Diffuse ischemic ST depression (subendocardial ischemia -- the epicardium is still perfused) always has reciprocal ST Elevation in lead aVR, as we see in this case. There is 1 mm STE in aVR. Remember aVR is calculated from leads I and II, and represents the OPPOSITE of a lead BETWEEN I and II. So a lead between I and II [call it (-) aVR] would have ST depression, while aVR has ST elevation.
So let's assume that the clinician established that this diffuse ischemia is indeed due to ACS:
This is not only severe coronary artery disease (CAD): the ECG and symptoms are both ACUTE, with active ischemia. Active ischemia is not a chronic condition; CAD is a chronic condition. So if this is indeed this is ACS, then there is severe CAD with plaque rupture and thrombus. People can have severe coronary disease, but if they have sudden chest pain and active ischemia, they have acute coronary syndrome. However, this is indeed not an OMI, because there is flow in the artery, but there is most likely thrombus with insufficient flow.
See these posts:
Does ST Elevation in lead aVR indicate acute coronary occlusion?
Diffuse ischemic ST depression (subendocardial ischemia -- the epicardium is still perfused) always has reciprocal ST Elevation in lead aVR, as we see in this case. There is 1 mm STE in aVR. Remember aVR is calculated from leads I and II, and represents the OPPOSITE of a lead BETWEEN I and II. So a lead between I and II [call it (-) aVR] would have ST depression, while aVR has ST elevation.
So let's assume that the clinician established that this diffuse ischemia is indeed due to ACS:
Are thrombolytics indicated for this acute coronary syndrome with ST depression?
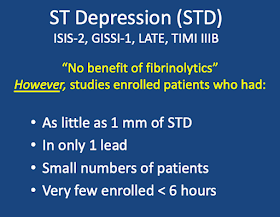
For years, ACS manifesting with ST depression was thought to NOT be an indication for thrombolytics. This was based on data from the early thrombolytic trials, as compiled in the FTT collaborative (Lancet 1994) which showed no benefit for groups with ST depression randomized to thrombolytics.
However, if you closely scrutinize those studies, only 4 of 9 studies in FTT enrolled patients with ST depression. Here is a summary, from my online lecture The False STEMI Non-STEMI Dichotomy:
However, there is plenty of data showing that mortality is high with increasing extent and depth (more millimeters in more leads) of ST depression. In fact, one year mortality is higher for patients with MI and ST depression than for those with ST Elevation:
It makes sense that, if there is thrombus in the artery causing active ischemia, even if not completely occlusive, lysing that thrombus might result in benefit (but of course only if recurrent thrombus formation is also prevented, which with thrombolytic therapy is done with concomitant administration of aspirin, clopidogrel 300 mg, and Heparin or enoxaparin).
However, no one has ever proven this in a randomized trial which limited patients to less than 6 hours, with at least 1-2 mm in at least 2 leads. It may very well be that with STD in I, II, aVF, and V3-V6, and STE in aVR, that thrombolytics would be proven beneficial.
In 2013, the ACC/AHA guidelines seem to have recognized this and changed the recommendation:
For years, ACS manifesting with ST depression was thought to NOT be an indication for thrombolytics. This was based on data from the early thrombolytic trials, as compiled in the FTT collaborative (Lancet 1994) which showed no benefit for groups with ST depression randomized to thrombolytics.
However, if you closely scrutinize those studies, only 4 of 9 studies in FTT enrolled patients with ST depression. Here is a summary, from my online lecture The False STEMI Non-STEMI Dichotomy:
However, there is plenty of data showing that mortality is high with increasing extent and depth (more millimeters in more leads) of ST depression. In fact, one year mortality is higher for patients with MI and ST depression than for those with ST Elevation:
It makes sense that, if there is thrombus in the artery causing active ischemia, even if not completely occlusive, lysing that thrombus might result in benefit (but of course only if recurrent thrombus formation is also prevented, which with thrombolytic therapy is done with concomitant administration of aspirin, clopidogrel 300 mg, and Heparin or enoxaparin).
However, no one has ever proven this in a randomized trial which limited patients to less than 6 hours, with at least 1-2 mm in at least 2 leads. It may very well be that with STD in I, II, aVF, and V3-V6, and STE in aVR, that thrombolytics would be proven beneficial.
In 2013, the ACC/AHA guidelines seem to have recognized this and changed the recommendation:
Here is the link to that. It is on page e95:
https://www.onlinejacc.org/content/accj/61/4/e78.full.pdf?download=true
This was a very surprising reversal of a long held recommendation AGAINST fibrinolytics for ST Depression. I believe it was appropriate. But I also think it should be much more qualified than they recommend because thrombolytics are potentially dangerous.
https://www.onlinejacc.org/content/accj/61/4/e78.full.pdf?download=true
This was a very surprising reversal of a long held recommendation AGAINST fibrinolytics for ST Depression. I believe it was appropriate. But I also think it should be much more qualified than they recommend because thrombolytics are potentially dangerous.
So this would be my management if no cath lab was available:
1. How unavailable is the cath lab? Is it 1 hour away, 2 hours, 3 hours? Totally unavailable?
2. How unstable is the patient? In shock or pulmonary edema? Then patients needs therapy immediately.
3. How deep and widespread is the STD?
4. Baseline risks? Age, baseline ejection fraction?
5. Risks of thrombolytic therapy? (Mainly what is the risk of intracranial bleeding?)
Furthermore, I would try to alleviate the ischemia with anti-ischemic, anti-platelet, and anti-thrombotic therapy:
1. I administer IV nitroglycerine, as much as the patient's blood pressure can tolerate.
2. Given antiplatelet agents, aspirin and clopidogrel (It is standard to give 300 mg clopidogrel with thrombolytics)
3. Given enoxaparin or unfractionated heparin
Then re-assess. Is the pain and ST depression resolved?
If the patient is still having severe ischemia, is high risk, does not have high risk for bleeding, and you are very far from an interventional hospital, then it is reasonable to give thrombolytics.
Finally, keep repeating the ECGs. The thrombus which is not occlusive can propagate and completely occlude the artery. Here is an example:





Very well written, however, I feel you should have mentioned the patients BP before discussing any further treatment options...
ReplyDeleteThanks for your comment! This was not my case — so I didn’t know all the details (I did not know what the BP was). As per Dr. Smith’s commentary — in addition to consideration of thrombolytic therapy (given lack of cath lab availability in this case) — anti-ischemic measures would be indicated (ie, “IV nitroglycerine, as much as the patient’s BP can tolerate”). Dr. Smith added important factors to consider in the decision-making process regarding whether to give thrombolytics (with of course it being imperative that there be no contraindications, such as uncontrolled hypertension — if thrombolytics were to be given).
DeleteThanks for sharing the case. I would like to know how to differentiate NSTEMI from pulmonary embolism in this ecg. Since there are several signs indicate RV strain or RV injury, including aVR STE, RBBB, RAD, S1Q3T3.
ReplyDeleteTHANKS for your comment. Hi. First — the finding of diffuse ST depression + ST elevation in aVR does not diagnose infarction — bur rather diffuse subendocardial ischemia that may be due to severe coronary disease (not necessarily infarction thought!) or to other cause that increase demand (ie, tachycardia, blood loss, sepsis, shock, etc.)
DeleteReasons I did not consider acute PE in this case include: — i) The history was 2 hours of new-onset chest pain. That sounds like coronary disease — and not acute PE; — ii) While true that new RBBB could be seen with acute PE — QRS morphology in lead V1 does not show a “neat” rSR’ complex, with S wave descending below the baseline, and slender R’ — but rather a qR pattern with slurring of the QRS complex. While not perfectly predictive — this pattern is more suggestive of someone who has underlying heart disease (possibly coronary disease) — and not sudden new onset of RBBB; — iii) ST depression in this tracing is diffuse — and in some leads (ie, V2, V3) we see a distinct shelf-like (flat) ST depression shape. This is NOT the pattern (shape) of RV strain. RV strain would look more like the shape of the ST-T depression that we see in lead V1 and lead III. RV “strain” should be seen most in anterior leads and inferior leads — and not diffuse in all leads as it is here; iv) RV strain gets less as you move to lateral leads; — v) There is no RAA (which is often seen in acute PE); and — vi) Rather than a “right axis” — there is RBBB. You are supposed to get a deep terminal S wave just because of the RBBB. And the S1Q3T3 that we see is often a “natural” part of a RBBB. So these ECG findings in association with a RBBB that looks like this one are not predictive of acute PE.
Great case and explanation. Did the patient get any thrombolytics ??. Any follow up's ?
ReplyDelete