Written by Pendell Meyers
(with really great and thorough explanation of this finding by Ken Grauer).
At my hospital, patients with any symptoms which could be vaguely interpreted as a possible stroke during the triage process are brought to the high acuity area and a provider is asked to do a "neuro check", which involves a quick H and P and exam to determine if we should activate our stroke protocol.
A man in his 70s was brought to me for a neuro check, and the triage providers commented that they were worried about a possible seizure as well. The patient was alert and oriented with normal vitals at triage. He stated that the last thing he remembers was sitting at his desk working on some paperwork, then he remembers being on the ground looking up at paramedics. His wife heard a noise and found him on the floor next to his desk. He could not recall feeling anything unusual prior to the event, was in good health earlier that day, and felt completely normal at the time of my evaluation with no complaints. Of note, he had an identical episode last week for which he did not seek medical attention.
So I asked for an ECG as syncope was high in the differential.
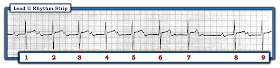
Here is his initial ECG:
Interpretation: Sinus rhythm with extreme 1st degree AV block (PR interval roughly 500 msec!)
There is a narrow, regular QRS which could arguably meet morphology criteria for LAFB. The ST segments and T-waves are normal, but they are followed immediately by another wave that at first may be confused in some leads (especially in lead II rhythm strip) for a U-wave. However, looking in all 12 leads reveals that this wave has textbook P-wave morphology (biphasic up-down in V1, upright in II). In addition, there is no other wave which could be a P-wave, therefore if it were a U-wave then the rhythm would have to be junctional (the computer mistakenly thought this was junctional rhythm by the way). The width of the P-wave and the "second bump" of the P-wave in lead II may suggest atrial enlargement, but this is not particularly relevant clinically in this case.
Assuming there are no extra P-waves hidden inside the QRS complexes (I don't see any), then there is a 1:1 relationship of P-waves to QRS complexes. There are no dropped beats, and the PR interval is not prolonging. This pattern has two possible etiologies:
1) Sinus rhythm with 1st degree AV block
2) Sinus rhythm with complete 3rd degree AV block, with a junctional rhythm that exactly matches the rate of the SA node (the two rhythms are dissociated due to the complete AV block, and the result is called "isorhythmic dissociation")
It is extremely unlikely that two separate, dissociated rhythms are at EXACTLY the same rate, and thus #1 is far more likely than #2. As this pattern persists for more and more time, the chances of isorhythmic dissociation (#2) approach zero.
So to be sure, I stood by the bedside and watched the cardiac monitor carefully for a few minutes. There was never a single dropped beat, and the PR interval never changed.
The diagnosis is sinus rhythm with 1st degree AV block, with extremely long PR interval.
All ECGs with bradycardia and/or heart block should be considered for hyperkalemia and inferior OMI (because the RCA supplies the SA and AV nodes) as a cause, but this ECG shows no evidence of these etiologies.
So what is the cause of the patient's event?
The most likely explanation is that he had transient 2nd or 3rd degree heart block resulting in bradycardia and decreased cardiac output leading to syncope. Between these episodes his ECG shows only first degree heart block as a clue of what happened.
We carefully reviewed his medications and found no beta blockers, calcium channel blockers, digoxin, or any other medications which could cause or contribute to bradycardia. We kept him on the cardiac monitor with pacer pads just in case, but never had to use them. His potassium returned normal, and his troponin negative. He had no further syncopal events. He was admitted to cardiology.
He received a pacemaker and is doing well so far.
Learning Points:
Any time seizure or syncope is on the differential, the other one is also on the differential.
1st degree AV block is defined as PR interval greater than 200 msec. Most cases are between 200-300 msec, with 500 msec (as in this case) being extraordinarily long.
Although 1st degree AV block is often inconsequential in the ED, it should be taken seriously when the patient has symptoms compatible with intermittent higher grade AV blockade. I am not aware of specific PR cutoffs that indicate especially high risk in asymptomatic patients.
Use all 12 leads to see more examples and morphologies of a wave to distinguish whether it is a P-wave with 1st degree AVB versus a U-wave.
Make sure to look for an extra set of P-waves hidden within the QRS complex.
When the P to QRS ratio is 1:1, isorhythmic dissociation is an unlikely possibility which becomes less and less likely as time goes on.
1st degree AV block is usually thought to be inconsequential, however in some cases it is an indicator of serious AV node disease and an indicator of intermittent higher-grade AV block.
In the emergency department, the most important etiologies of bradycardia and AV block are remembered by the mnemonic "DIE": Drugs (CCBs, BBs, digoxin, etc), Ischemia (usually of the RCA which supplies the SA and AV nodes), and Electrolytes (hyperkalemia).
Detailed ECG interpretation is vital in syncope. I personally use and teach the WOBBLER mnemonic.
(with really great and thorough explanation of this finding by Ken Grauer).
At my hospital, patients with any symptoms which could be vaguely interpreted as a possible stroke during the triage process are brought to the high acuity area and a provider is asked to do a "neuro check", which involves a quick H and P and exam to determine if we should activate our stroke protocol.
A man in his 70s was brought to me for a neuro check, and the triage providers commented that they were worried about a possible seizure as well. The patient was alert and oriented with normal vitals at triage. He stated that the last thing he remembers was sitting at his desk working on some paperwork, then he remembers being on the ground looking up at paramedics. His wife heard a noise and found him on the floor next to his desk. He could not recall feeling anything unusual prior to the event, was in good health earlier that day, and felt completely normal at the time of my evaluation with no complaints. Of note, he had an identical episode last week for which he did not seek medical attention.
So I asked for an ECG as syncope was high in the differential.
Here is his initial ECG:
 |
| What do you think? |
Interpretation: Sinus rhythm with extreme 1st degree AV block (PR interval roughly 500 msec!)
There is a narrow, regular QRS which could arguably meet morphology criteria for LAFB. The ST segments and T-waves are normal, but they are followed immediately by another wave that at first may be confused in some leads (especially in lead II rhythm strip) for a U-wave. However, looking in all 12 leads reveals that this wave has textbook P-wave morphology (biphasic up-down in V1, upright in II). In addition, there is no other wave which could be a P-wave, therefore if it were a U-wave then the rhythm would have to be junctional (the computer mistakenly thought this was junctional rhythm by the way). The width of the P-wave and the "second bump" of the P-wave in lead II may suggest atrial enlargement, but this is not particularly relevant clinically in this case.
Assuming there are no extra P-waves hidden inside the QRS complexes (I don't see any), then there is a 1:1 relationship of P-waves to QRS complexes. There are no dropped beats, and the PR interval is not prolonging. This pattern has two possible etiologies:
1) Sinus rhythm with 1st degree AV block
2) Sinus rhythm with complete 3rd degree AV block, with a junctional rhythm that exactly matches the rate of the SA node (the two rhythms are dissociated due to the complete AV block, and the result is called "isorhythmic dissociation")
It is extremely unlikely that two separate, dissociated rhythms are at EXACTLY the same rate, and thus #1 is far more likely than #2. As this pattern persists for more and more time, the chances of isorhythmic dissociation (#2) approach zero.
So to be sure, I stood by the bedside and watched the cardiac monitor carefully for a few minutes. There was never a single dropped beat, and the PR interval never changed.
The diagnosis is sinus rhythm with 1st degree AV block, with extremely long PR interval.
All ECGs with bradycardia and/or heart block should be considered for hyperkalemia and inferior OMI (because the RCA supplies the SA and AV nodes) as a cause, but this ECG shows no evidence of these etiologies.
So what is the cause of the patient's event?
The most likely explanation is that he had transient 2nd or 3rd degree heart block resulting in bradycardia and decreased cardiac output leading to syncope. Between these episodes his ECG shows only first degree heart block as a clue of what happened.
We carefully reviewed his medications and found no beta blockers, calcium channel blockers, digoxin, or any other medications which could cause or contribute to bradycardia. We kept him on the cardiac monitor with pacer pads just in case, but never had to use them. His potassium returned normal, and his troponin negative. He had no further syncopal events. He was admitted to cardiology.
He received a pacemaker and is doing well so far.
Learning Points:
Any time seizure or syncope is on the differential, the other one is also on the differential.
1st degree AV block is defined as PR interval greater than 200 msec. Most cases are between 200-300 msec, with 500 msec (as in this case) being extraordinarily long.
Although 1st degree AV block is often inconsequential in the ED, it should be taken seriously when the patient has symptoms compatible with intermittent higher grade AV blockade. I am not aware of specific PR cutoffs that indicate especially high risk in asymptomatic patients.
Use all 12 leads to see more examples and morphologies of a wave to distinguish whether it is a P-wave with 1st degree AVB versus a U-wave.
Make sure to look for an extra set of P-waves hidden within the QRS complex.
When the P to QRS ratio is 1:1, isorhythmic dissociation is an unlikely possibility which becomes less and less likely as time goes on.
1st degree AV block is usually thought to be inconsequential, however in some cases it is an indicator of serious AV node disease and an indicator of intermittent higher-grade AV block.
In the emergency department, the most important etiologies of bradycardia and AV block are remembered by the mnemonic "DIE": Drugs (CCBs, BBs, digoxin, etc), Ischemia (usually of the RCA which supplies the SA and AV nodes), and Electrolytes (hyperkalemia).
Detailed ECG interpretation is vital in syncope. I personally use and teach the WOBBLER mnemonic.
===================================
MY Comment by KEN GRAUER, MD (5/24/2020):
===================================
Interesting case presented by Dr. Meyers! The patient was a man in his 70s, who presented to the ED with possible syncope and an abnormal ECG. The following QUESTIONS were raised during Dr. Meyers’ discussion:
- HOW CAN WE TELL if the small upright deflection that we see after the T wave, and near the middle of each R-R interval is a P wave or a U wave?
- In ECG #1 — HOW can we rule out the possibility of complete (ie, 3rd-degree) AV block?
- Could there be “isorhythmic AV dissociation?” — in which atrial and AV nodal pacemakers manifest a nearly identical heart rate?
- Is the rhythm regular?
- HOW can calipers help you to rapidly answer the questions in the 4 bullets above this?
Exploration of this case also poses the following Clinical QUESTIONS:
- What is the clinical significance of 1st-degree AV block?
- How long can the PR interval be, and still conduct?
- Does 1st-degree AV block become more “dangerous” once the PR interval becomes “very” long? IF so — WHY?
My Comment below is aimed at providing another perspective at answering the above questions.
- For clarity — I’ve reproduced the initial ECG in this case in Figure-1:
 |
| Figure-1: The initial ECG in this case (See text). |
MY THOUGHTS: Did YOU think that the rhythm in ECG #1 was regular? Although easy to assume from rapid inspection that the rhythm in ECG #1 is regular — it is not regular!
- Using calipers will tell you within seconds that the rhythm in ECG #1 is not regular (Figure-2).
HOW to Distinguish P waves from U waves?
On occasion — it can be difficult to distinguish P waves from U waves. The KEY for making this distinction — is to determine IF the deflection in question is related to what comes before it (ie, to the QRS complex and T wave to the left of the deflection in question) — or, to what comes after it (ie, to the next QRS complex, that lies to the right of the deflection in question)?
- Using calipers — I carefully measured the PR interval before each beat in Figure-3.
- NOTE that the PR interval before each beat in Figure-3 remains constant ( = 460 msec). The fact that despite a changing R-R interval — the PR interval in Figure-3 remains constant, means that each of these P waves is conducting (albeit with marked 1st-degree AV block).
In contrast — the RP interval does not remain constant — as shown by the different RP interval durations that appear in PURPLE numbers in Figure-4.
- This means that each of the deflections under the RED arrows in Figure-4 must be related to the QRS complex ahead of it — and not to the QRS complex and T wave that came before ...
- This confirms that the deflections under the RED arrows in Figure-4 are P waves. IF they were U waves — then the R-"U" interval would be constant.
Why We Know the Rhythm in ECG #1 is Not 2nd- or 3rd-Degree AV Block?
We have established that each of the P waves in ECG #1 are conducting with an extremely prolonged PR interval (of 460 msec). But HOW can we rule out the possibility of some higher degree of AV block?
- PEARL #1 — Dr. Meyers showed us this “Pearl” — which is simply to observe the monitor for a period of time — until it becomes clear IF the rhythm is changing (ie, in this case — whether the relationship between each P wave and the next QRS complex to follow it, maintains the same PR interval of 460 msec).
- As per Dr. Meyers — it would be exceedingly unlikely for there to be isorhythmic AV dissociation without apparent change in the PR interval, for so many beats from simultaneously firing AV nodal and SA nodal pacemakers.
WHAT IS “Isorhythmic” AV Dissociation?
The general term of AV dissociation simply means, that for a certain period of time sinus P waves are not related to neighboring QRS complexes. That is, P waves preceding one or more QRS complexes are not being conducted to the ventricles.
- AV Dissociation may be intermittent, recurrent and/or short-lived — or — it may be complete and persistent/permanent, as occurs with 3rd-degree AV block.
- AV Dissociation is said to be “isorhythmic” — when there are 2 independent pacemakers (usually sinus P waves from the SA node and an accelerated junctional focus) — with these 2 pacemaker sites having identical (or nearly identical) rates. In Figure-5 — a “picture” tells 1,000 words.
NOTE: True “isorhythmic” AV dissociation is like a horse race — in that rather than persistent near-equal rates for SA nodal and AV nodal pacemakers — there is a given-and-take — with first one horse (ie, one pacemaker) taking the lead by a tiny amount — then the other horse (ie, the other pacemaker) taking back that ever-so-slim margin of lead — and back-and-forth.
- This back-and-forth can be seen in Figure-5 — in which there is an ever-so-slight-but-real change in both the sinus and accelerated AV nodal escape rate. As a result — the PR interval in Figure-5 continually changes from beat-to-beat.
- In contrast — the relationship in Figure-4 between P waves and the next QRS complex remains the SAME (ie, the PR interval remains constant = 460 msec) in ECG #1.
- PEARL #2 — AV dissociation is never a “diagnosis”. Instead — it is a condition caused by “something else”. There are 3 Causes of AV Dissociation: i) AV Block itself (of 2nd- or 3rd-degree); ii) Usurpation — in which P waves transiently do not conduct because an accelerated junctional rhythm takes over (ie, “usurps” control of the rhythm); and, iii) Default — in which a junctional escape rhythm takes over by “default” (ie, because of SA node slowing) — as may occur if a medication such as a ß-blocker is being used.
- The task for the clinician is to figure out what the cause of AV dissociation is for any given rhythm. This task is far more than academic — since appropriate management depends on figuring out the cause of AV dissociation. Active treatment may or may not be indicated. For example — optimal treatment of complete AV dissociation by “usurpation”, say with an accelerated junctional rhythm due to digitalis toxicity is simple: Stop digoxin!
- PEARL #3 — Complete AV Dissociation is not the same as 3rd-degree AV block! This is one of the most commonly misunderstood concepts in all of arrhythmia interpretation! Complete AV block is just one of 3 possible causes of AV dissociation. Patients with “complete AV dissociation” may actually have no degree of AV block at all. This is the case in Figure-5 — in which after beat #1, none of the other 8 P waves in this tracing are conducted. But since none of these 8 P waves ever has a chance to conduct (ie, because the PR interval preceding beats #2-thru-9 is too short to conduct) — we have NO WAY of knowing whether P waves could conduct IF given the chance! Thus, the correct diagnosis for the rhythm in Figure-5 is not “AV dissociation” — but rather, “Sinus rhythm with AV dissociation as a result of “usurpation”, produced by a slightly accelerated junctional pacemaker at 74/minute”.
- PEARL #4 — Complete (or 3rd-degree) AV Block is said to be present when none of the impulses from above (P waves) are able to conduct to the ventricles. KEY to this definition is the need to demonstrate that P waves fail to conduct despite being given adequate opportunity to do so — which requires that we must see P waves occurring in all phases of the R-R cycle (ie, having opportunity to conduct — but failing to do so). Note that none of the 8 P waves that fail to conduct in Figure-5 have any “chance” to conduct — which is why we are unable diagnose any degree of AV block from this particular tracing.
- PEARL #5 — Most of the time, IF the degree of AV block is complete (3rd-degree) — then the ventricular rhythm should be at least fairly regular. This is because escape rhythms arising from the AV node, the His or ventricles are usually fairly regular rhythms. Exceptions may occur (ie, during cardiopulmonary resuscitation) — but even then, there will usually be a recognizable pattern of ventricular regularity. Going BACK to Figure-2 — the obvious irregularity of the ventricular rhythm (R-R interval varying from 800-to-930 msec) is yet another clue telling us that complete AV block is highly unlikely for ECG #1!
- IF interested in more on “My Take” of the Basics of AV Block — CLICK HERE. To go directly to the section that distinguishes AV Dissociation from Complete AV Block — CLICK at 49:25 in the video.
PEARLS about 1st-Degree AV Block:
Today’s case brings up a series of concepts regarding 1st-Degree AV Block:
- Traditionally — the diagnosis of 1st-degree AV block is defined as a PR interval of more than 0.20 second (ie, clearly more than 1 LARGE box in duration on ECG grid paper). That said — some individuals normally have PR intervals slightly above this upper range. This is especially true for athletic young adults, who often manifest increased vagal tone. As a result — I prefer the PR interval to be at least 0.22 second before saying 1st-degree AV block is present.
- Norms for the PR interval are different in children. Pediatric hearts are smaller. It therefore takes less time for the electrical impulse to travel through the conduction system of a child. For example — a PR interval of 0.18 second would be long for an infant.
- In younger adults — the cause of 1st-degree AV block is often the result of increased vagal tone. This can be a “training effect” — that goes way on deconditioning. In contrast — the causes of 1st-degree AV block in an older adult include fibrosis (aging) of the conduction system; coronary disease; myocarditis; rheumatic fever; infiltrative disease, Lyme disease; and neuromuscular disorders.
- The PR interval is defined as “short” — if it measures less than 0.12 second in lead II (as may occur with WPW when the AV node is bypassed). That said — some patients may normally have a PR interval slightly less than 0.12 second without necessarily having an accessory pathway (they may have an anatomically small AV node — or more-rapid-than-usual conduction through the AV node).
- HOW LONG can the PR interval be and still conduct to the ventricles? The answer is very long! I have seen PR intervals of greater than 1.0 second that still conduct to the ventricles in association with Mobitz I AV block.
- Clinically — Most patients with 1st-degree AV block remain asymptomatic and without need for intervention. This is especially true when the severity of 1st-degree AV block is not great (ie, a PR interval less than 0.30 second). Once the PR interval extends beyond 0.30 second — the delay in ventricular contraction that occurs may result in the atria contracting against closed AV valves, with reduction in cardiac output. This may lead to a series of symptoms similar to “pacemaker syndrome” (ie, dizziness, fatigue, light-headedness, presyncope/syncope, dyspnea and/or chest pain).
- On occasion — implantation of a permanent pacemaker may be needed in patients with marked 1st-degree AV block (ie, PR interval significantly greater than 0.30 second) who are symptomatic as a direct result of PR interval prolongation. This apparently is what happened in today's case — in which this man in his 70s presented with suspected syncope + a markedly prolonged PR interval of ~460 msec.
- Bottom Line: While the vast majority of patients with 1st-degree AV block are asymptomatic and do well without need for treatment — it is important to be aware of cardiac and other underlying disorders that the patient may have, as these may influence prognosis. As patients become older — 1st-degree AV block may progress to more prolonged PR interval prolongation, more advanced degrees of AV block and/or development of atrial arrhythmias including AFib. An occasional patient who presents with marked 1st-degree AV block + symptoms directly due to this, may need pacemaker placement.
- For a concise Review of 1st-Degree AV Block that appeared in NCBI StatPearls, 2019 — CLICK HERE.
Finally — Consider the rhythm shown in Figure-6. WHAT is going on?
- Can YOU guess WHY I am showing the rhythm in Figure 6 in this post that deals with 1st-degree AV block?
 |
| Figure-6: WHAT is going on in this rhythm? (See text). |
INTERPRETATION of Figure-6: The rhythm is fairly regular — except for a brief pause after beat #7. The QRS complex is narrow — and P waves appear to be present. Can YOU identify all of the P waves?
- HINT: Using calipers should make it much easier to spot all of the P waves!
Identifying P Waves in Figure-6: I’ve added RED arrows in Figure-7 to highlight the location of all of the P waves:
- The atrial rhythm is actually quite regular at a rate of ~60-65/minute (RED arrows).
- Note that a P wave is hidden within the T wave of beat #6. The P wave that follows is more obvious — because it produces a spike in the T of beat #7.
- Final PEARL: This is a long Wenckebach cycle! On occasion with 2nd-degree AV block, Mobitz Type I ( = AV Wenckebach) — there will be a long series of beats before one is dropped. For example, in Figure-7 — it is difficult to appreciate that the PR interval is increasing as one moves from beat #2 — to beats #3, 4, 5, and 6. This is because the cycle of beats until one is dropped is long — and, the PR interval “increment” between one beat and the next is small. In such cases — the KEY that allows rapid identification of Mobitz I is to measure the PR interval at the beginning of the run (ie, the PR interval of beat #1) — and compare it to the PR interval at the end of the run just before the dropped beat. It should now be obvious that the PR interval of beat #7 is clearly much longer than the PR interval of beat #1. And then with the next cycle — the PR interval of beat #8 again shortens.
- P.S.: IF you'd like another Case Study on this phenomenon — CHECK OUT my ~11-minute ECG Video on this subject.
Our THANKS to Dr. Meyers for presenting this interesting case!






The rhythm is not entirely regular, as Dr. Grauer identifies. On several beats there are differences in the P-P and R-R intervals. The P-P interval changes precede and predict the R-R interval changes. This proves that the atria and ventricles are associated (specifically, with A driving the V).
ReplyDeleteThe changes in sinus rate likely represent simple sinus arrhythmia/respiratory variation.
The patient's clinical symptoms of several minutes LOC (I'm assuming EMS took at least a few minutes to get there) do not fit as well with an arrhythmic syncope (which would usually last a few seconds only). May have had a concussion from the fall causing memory loss, though. Pacing is reasonable with such severe PR prolongation, nonetheless. EPS for risk stratification could be done to prove it is infranodal if one wanted to avoid pacemaker implantation.
@ Emart — THANK YOU for your comment. This was not my case — so I do not know details. All we are told is that, “He received a pacemaker and is doing well so far”. I did not see from the abbreviated history we received, suficient indication for permanent pacing. This is NOT to say that there was no such indication — but rather to acknowledge that it is NOT common for pacing to be needed for 1st degree AV block. That said — the important “Take Home” Point from this excellent case, is that the PR interval WAS greatly prolonged — and that IF hospital observation did verify symptomatic bradycardia and/OR symptomatic problems shown to be a direct result of the prolonged PR interval (ie, atrio-ventricular asynchrony) — then YES, permanent pacing would be indicated. Would be nice to know the specifics that were discovered during hospital stay to lead to the decision for pacing. THANKS again for your comment! — :)
DeleteVery interesting (and rare!) ECG. And a great discussion by Pendell and Ken. It's amazing how many ECG books even today still define 3rd degree AV block by AV dissociation alone. As (I think) Marriott said (and I paraphrase him), "It's not the varying PR intervals that define 3rd degree AV block; it's the P waves that should have conducted... but didn't."
ReplyDeleteOne aspect to consider is that when you have a first degree AV block this profound, it takes very little increase in the atrial rate to make atrial systole coincide with ventricular systole. This can result in a sudden decrease in cardiac output and syncope because the atria will be contracting against closed AV valves. If the patient also happens to have COPD it can cause marked respiratory distress.
My impression from this presentation is that no advanced AV block or tachydysrhythmia was ever observed or recorded.
First degree AV block is very, very infrequent in people under the age of 35 years or so and gradually becomes more evident with age - but 500 msec is way too much! Was the patient checked for Lyme disease? Most permanent 3rd degree AV blocks occur below the AV node, so I think the cardiologists probably inserted a dual chamber pacemaker (set to AVI mode) to shorten the AV interval so that if the atrial rate increases a bit, the two systoles won't impinge on each other. First degree AV block can also occur below the AV node, but since the QRS complexes here are normal and narrow, that would require equal delay in the right and left bundle branches, which is about as likely as a perfect isorhythmic AV dissociation that persists for hours. And so many people still think that first degree AV block is always benign and never requires treatment. Here we have a first degree AV block that required a pacemaker.
The mean QRS axis is a bit confusing. The QRS with the greatest magnitude in the frontal plane is in Lead III. Because the S in III > R in aVL, that puts the mean QRS axis between the two but closer to the negative pole of Lead III located at -60 degrees. That is definitely a LAFB since it is greater than -45 degrees. However, Lead II is almost exactly equiphasic which should move it closer to -30 degrees. I'm not sure how to explain that. Lead II really should have an rS morphology. The LAFB explains the clockwise rotation in the precordial leads with the terminal QRS vector pointing so far to the left.
THANKS (as always!) for your comment Jerry. As per my answer just now to Emart (just above your comment) — I don’t know details from the hospital stay … Would have been nice to know exactly what transpired — and WHAT was the info obtained that led to the decision for permanent pacing. Also, as you mention (and I mentioned in my 3rd bullet under Pearls about 1st Degree AV Block) — a KEY point is to try to determine the etiology of the 1st Degree (especially given how marked PR prolongation is here).
DeleteAs to the mean QRS axis in my ECG #1 — I calculated it at right around -30 degrees (taking account net deflections in the 3 standard limb leads — and accounting for the net area in the positive R wave in II being about equal to the net negative area in this lead). Having read everything I could on the subject of hemiblocks before deciding many years ago on how to define “LAHB” in my ECG interpretation books — I evolved to the impression that the experts don’t agree on definite criteria — and that “life can be simpler” by using lead II as my “decider” when there is LAD (left axis deviation). IF the net QRS deflection in lead II is clearly more negative than positive — I’ve found that to be a reliable indicator of LAHB (that can be determined in less than 5 seconds by even intermediate interpreters — and which I’ve found to be as accurate as anything described by expert electrocardiographers). I would NOT have called LAHB in this example — because the net deflection (counting area under the curve) in lead II is not clearly more negative than positive. I realize you and others may have different approaches to this issue — and all viewpoints are welcome! THANKS again Jerry! — :)
Thank you so very much.
ReplyDeleteOur pleasure Polly! THANKS for your interest! — :)
DeleteThank you so very much.
ReplyDeleteOur pleasure Polly! — :)
Delete