The medics were called for sudden LOC and then awakening, witnessed by his spouse.
The patient looked ill to them.
They recorded a prehospital ECG, which is not available but looked like the ED ECG.
Based on that prehospital ECG, they activated the cath lab:
On arrival the patient was well appearing and asymptomatic, fully recovered. Thus the symptoms is syncope. (only when someone is fully recovered can it be called "syncope").
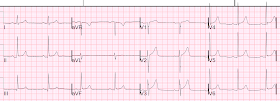
ECG:
ST elevation in II, III, aVF, V2-V4, and V5, V6. There is no reciprocal ST depression in aVL.
If the patient had chest pain, many would diagnose pericarditis.
But this is a completely normal ECG. The ST Elevation is normal.
I did not know about the patient's clinical condition, but was shown this ECG and I said, "this ECG is not an indication for the cath lab. You should cancel it unless there is some compelling clinical reason to go."
Activating the cath lab is a clinical decision, and if you think the patient has OMI, the you should do so "regardless of ECG or biomarker findings" (European NSTEMI guidelines).
But cath lab activation should not be based upon this ECG. It is normal. (Of course an OMI may be present even with a normal ECG).
Syncope without other symptoms is very seldom due to OMI.
The patient was taken to the cath lab and had open coronaries. He ruled out for MI and was diagnosed with vasovagal syncope.
The patient looked ill to them.
They recorded a prehospital ECG, which is not available but looked like the ED ECG.
Based on that prehospital ECG, they activated the cath lab:
 |
| What do you think? |
On arrival the patient was well appearing and asymptomatic, fully recovered. Thus the symptoms is syncope. (only when someone is fully recovered can it be called "syncope").
Emergency Department Syncope Workup: After H and P, ECG is the Only Test Required for Every Patient.....
ECG:
ST elevation in II, III, aVF, V2-V4, and V5, V6. There is no reciprocal ST depression in aVL.
If the patient had chest pain, many would diagnose pericarditis.
But this is a completely normal ECG. The ST Elevation is normal.
I did not know about the patient's clinical condition, but was shown this ECG and I said, "this ECG is not an indication for the cath lab. You should cancel it unless there is some compelling clinical reason to go."
Activating the cath lab is a clinical decision, and if you think the patient has OMI, the you should do so "regardless of ECG or biomarker findings" (European NSTEMI guidelines).
But cath lab activation should not be based upon this ECG. It is normal. (Of course an OMI may be present even with a normal ECG).
Syncope without other symptoms is very seldom due to OMI.
The patient was taken to the cath lab and had open coronaries. He ruled out for MI and was diagnosed with vasovagal syncope.
===================================
Comment by KEN GRAUER, MD (6/7/2019):
===================================
It’s good to mix in normal tracings among the many subtle OMI ECG cases that are so often presented on this Blog. Recognizing what constitutes a “normal tracing” in a patient who summons EMS can be as equally challenging as detecting the early signs of acute OMI:
- POINT #1 — My “starting point” is always the History. As the Attending charged with overreading all ECGs for 35 medical providers in an ambulatory care clinic over a 30-year period — I found knowing the history of invaluable assistance for predicting the likelihood that abnormal-looking tracings in the “In-Box” on my desk were possibly acute vs probably without acute change.
- While obvious that the prevalence of acute ischemia is clearly much higher for ECGs obtained on the scene by EMS or from symptomatic patients who present to an ED (compared to an ambulatory care center) — it should be emphasized that the history in this case was that of a syncopal episode, and not of a patient with new chest pain! While lack of chest pain clearly does not rule out the possibility of acute OMI — it does lower the prevalence for finding acute ischemia in this type of patient.
In the hope of enhancing Dr. Smith’s above comments as to why the ECG in this case is not suggestive of acute OMI (and why acute cath lab activation need not be implemented on the basis of this ECG) — I thought it would be helpful to compare this June 7 tracing with the initial ED ECG taken from our previous case from June 4 (Figure-1).
 |
| Figure-1: The initial ECG in this case (TOP) — compared to the initial ECG in the ED from the Case of June 4 (See text). |
===================
MY Thoughts on the June 7 ECG: As per Dr. Smith — there is slight-but-real ST elevation in multiple leads (leads II, III, aVF; V2-thru-V6).
- The shape of this ST elevation is uniformly concave-up in each of these 8 leads (similar to the shape of the gently curved blue lines in leads V2, V3, V4). While this shape by itself does not rule out the possibility of acute ischemia — this type of ST segment shaping, when it occurs in association with no more than the small amount of ST elevation we see here + J-point notching (PURPLE arrows in V4, V5, V6) — is much more often associated with repolarization variants than acute ischemia.
Other features against this TOP tracing in Figure-1 representing acute ischemia include the following:
- Lack of any reciprocal ST depression (as emphasized by Dr. Smith).
- Completely normal R wave progression.
- All q waves seen in this tracing are small and narrow. Normal “septal” q waves (attributable to the normal left-to-right initial vector of septal activation) may commonly be seen in any of the lateral leads (seen here in leads V4,V5,V6). Normal “septal” q waves may also normally be seen in one or more inferior leads when the frontal plane axis is relatively vertical, as it is here.
- Lack of Localization! Note that the ST elevation described for this TOP tracing in Figure-1 is seen in numerous lead areas (ie, in inferior, anterior, and lateral chest leads). Acute ischemic heart disease is far more likely to localize — instead of manifesting the nearly identical appearance for the ST-T waves that we see here in 8 of the 12 leads in this tracing.
NOTE: None of these ECG features that I describe are perfect — and, additional assessment might be needed (ie, more history; serial tracings; stat Echo; troponin, etc.) before full comfort can be attained that no acute ischemic event is ongoing — but, the above described features taken together — in association with a history that does not include chest pain — strongly suggests that acute cath lab activation is not indicated on the basis of the TOP tracing in Figure-1!
====================
Comparison to the June 4 Case: I thought comparison between the ECG in this June 7 case — and the initial ECG obtained in the Case from June 4 explains better than words why I was immediately concerned about the BOTTOM (June 4) tracing in Figure-1, but not about the TOP (June 7) tracing.
- The History for the June 4 Case was new-onset and severe chest pain. There was no history of chest pain for the patient in the June 7 Case.
- As explained in detail in My Comment on the June 4 Case — there are a number of leads in this June 4 case that show definite and acute ST-T wave abnormalities. Proportionally (ie, compared to QRS amplitude) — the amount of ST elevation in lead aVF in the June 4 tracing is profound ( = about 50% of the amplitude of the tiny QRS in this lead). Note how “fat” the T wave in lead aVF is at its peak — and, how broad the T wave base is in this lead. A similar (albeit less marked) ST-T wave appearance in lead III + reciprocal ST depression in lead aVL in the June 4 case confirm acuity of the hyperacute ST-T wave in lead aVF. In contrast — none of the 8 leads showing ST elevation in the TOP (June 7) tracing manifest a fatter-than-expected T wave peak or broader-than-expected T wave base.
- Note straightening of the ascent of the ST-T wave in leads V1, V2 and V3 of the June 4 Case (parallel RED lines in these leads). Thus, the normal, upward-sloping concavity of the ST segment has been lost! As explained in My Comment on the June 4 Case — the clearly abnormal ST elevation in lead V1 (that is simply not seen in a normal ECG) confirms that this ST segment straightening in leads V1, V2 and V3 is a real-and-acute finding.
FINAL THOUGHT: Appreciation of abnormal-shape ST-T wave abnormalities in the context of assessing all 12 leads on an ECG defies numerical breakdown. The clinician simply needs to experience thousands of ECGs over time, with careful assessment and meticulous follow-up to learn which tracings turned out to be acute, and which were not. Even then — none of us are perfect in our interpretations. That said, attention to comparative features in the June 4 and June 7 ECGs as described above will helpfully assist in the process.
- Our THANKS to Dr. Smith for presenting this case.

Sir Could it be the syncope due to symptomatic bradycardia caused by some drug or sinus node disease.
ReplyDeleteIt was vasovagal syncope by careful history
DeleteWhat about t>r in v2 and positive t wave in v1? Are those normal in BER?
ReplyDeleteBoth of those are often found in BER. Read my article in which I derive and validate the formula. Lots of info on BER: https://www.annemergmed.com/article/S0196-0644(12)00160-6/fulltext
DeleteGreat teaching case, Steve - for everyone. In my classes, the participants spend a lot of time interpreting complex ECGs in front of the class with me guiding and sometimes challenging them. I always mix in some normals like this one. One of the participants asked why I included so many normals when she was there to learn complex, abnormal ECG interpretation. My response was, "If it's so easy to diagnose a normal ECG, why did it take you almost 3 minutes to conclude that it was normal?"
ReplyDeleteThere are as many kinds of "normal" ECGs as abnormal. Being able to recognize all the nuances of "normal" is essential.
GRAN ELECTROCARDIOGRAMA, EN EFECTO PODRÍA DIAGNOSTICARSE TAL VEZ PERICARDITIS SI TUVIERA DOLOR, COMO NOTA PARA DIFERENCIAR REPOLARIZACION PRECOZ DE PERICARDITIS ES; EN LA REPOLARIZACION PRECOZ POR EL MÉTODO DE GRANT EL VECTOR DEL SEGMENTO ST SE SITUA ENTRE 70° A 90 ° A LA DERECHA DEL VECTOR DE LA ONDA T, Y EN LA PERICARDITIS EL VECTOR DEL ST SE SITUA ENTRE 0° A 30° A LA IZQUIERDA DEL VECTOR DE LA ONDA T, IGUAL AYUDA QUE EN LA PERICARDITIS NORMALMENTE LA RELACIÓN DE AMPLITUD DEL SEGMENTO ST ENTRE LA ONDA T (ST/T) ES MAYOR DE 0.15. GRAN ELEECTROCARDIOGRAMA
ReplyDeleteIt is far more likely to be normal variant, as that is far more common. Moreover, there was neither a rub or an effusion. Only significant PR depression or low voltage T-waves should sway one away from normal towards pericarditis. When the ECG can be both normal or pericarditis, it should be read as pericarditis because that is far more common. So these are the indicators of pericarditis: rub, effusion, Large PR depression, small T-waves (high ST/T ratio)
DeleteYa que tiene una repolarizacion precoz tipo 2,se ha visto que se asocia a sincopes Y fibrilacion ventricular, no seria adecuado que sea valorado por electrofisiologia para estratificar su riesgo a futuro y probable marcapasos? gracias por su respuesta.
ReplyDeleteNot necessarily
Delete