This ECG, recorded in triage, was shown to me immediately, with no other info.....
I said:
"Inferior OMI (Occlusion Myocardial Infarction - see the Manifesto). Activate the cath lab."
Dr. Laura Schrag also saw this immediately and that is why she showed it to me.
Then I asked: "Chest pain? Is it a good story?"
Answer: The patient was a 60-ish woman with 3 risk factors who had had stuttering chest pain for a week, now constant.
What makes this diagnostic of OMI when there is less than 0.5 mm of ST Elevation?
--ST elevation is large relative to QRS size (the QRS above is very small)
--"Bulky" T-waves
--Absence of upward concavity of ST segments (which is what makes the T-wave bulky)
--Reciprocal ST depression in aVL
--Down-up T-wave in V2 (indicative of posterior MI)
A note on specificity of these findings:
I post here a lot of subtle OMI ECGs that people show me or send me. I do not show enough subtly NEGATIVE cases. The vast majority of cases that are texted to me or showed to me in real time, that physicians are worried about, I tell them: "This is not worrisome. Do NOT activate the cath lab." I always add: "The ECG can be normal in the setting of OMI, so I cannot say that there is no OMI; I can only say that it does not show on the ECG. If you are worried, then get serial ECGs, echo, etc."
But in this case, it definitely shows, and the findings are VERY specific. In this case, the interventionalist (a great guy and friend of mine) wrote in his note "Nonspecific ST changes." Many or most physicians would call these "Nonspecific ST-T abnormalities." But these are most definitely NOT "Non-diagnostic" findings. These are not "Non-specific."
She was taken to the cath lab and had a 95% hazy RCA lesion that was stented.
Here is the post PCI ECG:
Here are a bunch of ECGs with inferior ST Elevation that is NORMAL (normal variant STE):
I repeat:
You can see from the below ECGs that normal ST elevation may be very elevated, whereas the case above has hardly any ST elevation. It is features OTHER THAN ST ELEVATION which mark the above as acute MI, and the below as NOT acute MI.
Here are the features of OMI vs. normal STE:
--ST elevation is large relative to QRS size (the QRS above is very small)
--"Bulky" T-waves
--Absence of upward concavity of ST segments (which is what makes the T-wave bulky)
--Reciprocal ST depression in aVL
--Down-up T-wave in V2 (indicative of posterior MI)
 |
| What do you think? Computer read is: "Moderate ST depression" |
I said:
"Inferior OMI (Occlusion Myocardial Infarction - see the Manifesto). Activate the cath lab."
Dr. Laura Schrag also saw this immediately and that is why she showed it to me.
Then I asked: "Chest pain? Is it a good story?"
Answer: The patient was a 60-ish woman with 3 risk factors who had had stuttering chest pain for a week, now constant.
What makes this diagnostic of OMI when there is less than 0.5 mm of ST Elevation?
--ST elevation is large relative to QRS size (the QRS above is very small)
--"Bulky" T-waves
--Absence of upward concavity of ST segments (which is what makes the T-wave bulky)
--Reciprocal ST depression in aVL
--Down-up T-wave in V2 (indicative of posterior MI)
A note on specificity of these findings:
I post here a lot of subtle OMI ECGs that people show me or send me. I do not show enough subtly NEGATIVE cases. The vast majority of cases that are texted to me or showed to me in real time, that physicians are worried about, I tell them: "This is not worrisome. Do NOT activate the cath lab." I always add: "The ECG can be normal in the setting of OMI, so I cannot say that there is no OMI; I can only say that it does not show on the ECG. If you are worried, then get serial ECGs, echo, etc."
But in this case, it definitely shows, and the findings are VERY specific. In this case, the interventionalist (a great guy and friend of mine) wrote in his note "Nonspecific ST changes." Many or most physicians would call these "Nonspecific ST-T abnormalities." But these are most definitely NOT "Non-diagnostic" findings. These are not "Non-specific."
She was taken to the cath lab and had a 95% hazy RCA lesion that was stented.
Here is the post PCI ECG:
 |
| All STE is gone. T-waves have normalized, or inverted in lead III. |
Here are a bunch of ECGs with inferior ST Elevation that is NORMAL (normal variant STE):
I repeat:
You can see from the below ECGs that normal ST elevation may be very elevated, whereas the case above has hardly any ST elevation. It is features OTHER THAN ST ELEVATION which mark the above as acute MI, and the below as NOT acute MI.
Here are the features of OMI vs. normal STE:
--ST elevation is large relative to QRS size (the QRS above is very small)
--"Bulky" T-waves
--Absence of upward concavity of ST segments (which is what makes the T-wave bulky)
--Reciprocal ST depression in aVL
--Down-up T-wave in V2 (indicative of posterior MI)
Widespread ST Elevation. Activate the Cath Lab?
Cases 2 and 3.
Case 2
Case 3.
 |
| This was a false positive cath lab activation. It is clearly not an OMI. |
Cases 4. and 5., at the bottom of this post:
Case 4.
Case 5.
Case 6.
Case 7.
Case 8. At the bottom of this post.
-----------------------------------------------------------
Comment by KEN GRAUER, MD (10/14/2018):
-----------------------------------------------------------
Important blog post by Dr. Smith — which provides instant support of his October 9, 2018 post, in which we highlighted the importance of the Triage ECG interpreted by a capable clinician skilled in ECG interpretation (despite several published papers to the contrary).
- I focus my comments here on some additional fine points confirming why the initial ECG in this case (recorded in triage) — is definitive for OMI (Figure-1):
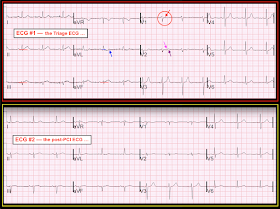 |
| Figure-1: Comparison between the initial triage ECG in this case (TOP) — with the post-PCI ECG (BOTTOM) after reperfusion of a high-grade RCA stenosis (See text). |
=========================
ECG #1 = the initial Triage ECG (TOP) — I repeat below (and illustrate in Figure-1) points made by Dr. Smith above, as well as some additional points:
- QRST amplitude in the inferior leads is often quite modest. As a result, OMIs may not declare themselves by as much ST elevation as is written into some “guidelines”. Instead, ST-T wave SHAPE takes on prime importance — as well as integration into our “Gestalt analysis” of the relative amount of ST-T wave deviation in cases when there is no more than modest QRS amplitude.
- There is debate among clinicians as to whether the PR or TP segment baseline should be used to assess the amount of ST segment deviation (Figure-2). BOTH are potentially correct — depending on the case at hand. There may be significant artifact or baseline wander that blurs definition of what constitutes the “baseline” in any given tracing. I prefer the PR segment baseline in those tracings in which this landmark is distinct — keeping in mind that the PR segment typically shortens (and is not always straight) as heart rate increases. Other clinicians prefer the TP baseline. SUGGESTION: Be open to using either the PR or TP segment as your “baseline” — and sometimes (when there is lots of artifact/baseline wander) using your “Gestalt average” of the two when neither is clear. (CLICK HERE — for the source of Figure-2).
 |
| Figure-2: Use of either the PR or TP segment to determine the “baseline” (See text). |
Continuing with our discussion of the subtle ECG changes in Figure-1:
- There is significant baseline artifact in Figure-1. That said, I believe we still can confidently determine the baseline. I’ve drawn in RED horizontal lines that correspond to the PR segment baseline. Based on these — there is ST elevation in each of the 3 inferior leads. The relative amount of this ST elevation is ~50% of the height of the tiny r waves in leads III and aVF, which most definitely is clinically significant!
- NOTE: Even if you selected the TP baseline instead of the PR baseline — there still is ST elevation with straight takeoff of the ST segment, and hyperacute-appearing T waves in each of the 3 inferior leads in ECG #1 of Figure-1.
- Although subtle — there is some ST depression in lead aVL (ie, the ST segment in this lead clearly dips below the horizontal BLUE PR segment baseline). In addition, there is terminal positivity of the T wave in lead aVL (BLUE arrow) — which correlates well with acute OMI.
- Dr. Smith emphasized the “down-up” T wave in lead V2 as strongly suggesting associated acute posterior infarction. This finding is subtle, but real! For clarity — I’ve drawn in a PINK arrow over the initial negative portion of this T wave — and a PURPLE arrow over the terminal positivity. (NOTE: This is the same phenomenon I just described with the BLUE arrow in lead aVL).
- The ST-T waves in leads V3-thru-V5 are also clearly abnormal! Note straightening of the short ST segment (especially in V3,V4) prior to abrupt rise to a taller-than-expected symmetric T wave (especially in V3,V4). I interpret these findings as further support of associated ongoing acute posterior infarction.
- Finally — I believe there is subtle-but-real ST elevation in lead V1 — or at-the-least ST segment coving in this lead that is not typically seen (RED arrow within the RED circle in V1). In the setting of an ECG suggesting acute RCA occlusion — this suggests probable acute RV involvement (thought right-sided leads would be needed to confirm this).
- NOTE: This makes for a total of 9/12 leads on the triage ECG ( = ECG #1) that show subtle-but-real acute ST-T wave findings. This is the BEST way to confirm OMI — namely that acute findings (even if subtle) are found in so many leads!
==================
ECG #2 = the post-PCI ECG (BOTTOM) — Confirmation of each of the findings I cite above is forthcoming from comparison of ECG #1 with the 2nd ECG in this case, obtained after reperfusion.
- FIRST — Note that there has been a change in frontal plane axis in ECG #2. This is important to appreciate, because we need to take into account the different QRS appearance when assessing ST-T wave changes (ie, there is now LAHB). That said, I believe lead-by-lead comparison in both limb and chest leads between ECG #1 and #2 does provide valid indication of what has changed.
These are the differences I note between ECG #1 and #2:
- ST elevation in the inferior leads has resolved.
- ST depression has resolved in aVL.
- ST coving with slight elevation is no longer present in V1.
- The biphasic T wave in V2 is gone (the T is purely positive now).
- Leads V3-thru-V5 now look normal. Note that the ST segment prior to onset of the T wave in V3 and V4 now shows normal gradual upsloping (instead of ST segment straightening) — and the T waves in these leads are smaller and less symmetric than they were in ECG #1.
LEARNING POINT: The BEST way to hone your ECG interpretation skills is to regularly compare pre- and post-reperfusion tracings — to see what has changed! This confirms that subtle initial abnormalities were real — and makes you better the next time at recognizing subtle-but-important ECG findings from the start.
- Our THANKS to Dr. Smith for this highly instructive case!








I always learn so much from you. Thank you for posting these cases and especially for posting the normal ones too.
ReplyDeleteDr. Smith, I want to ask you a question regarding to LAFB. As I have read, the left anterior fascicular is mainly supplied by left coronary artery, so why in this case inferior MI due to RCA occlusion can cause LAFB?
ReplyDeleteThis case does NOT have LAFB, but if it did, it would not be caused by the inferior MI, but would be pre-existing.
DeleteThank you sir.
DeleteHi Dr Smith,
ReplyDeleteAs a pre-hospital provider I often don't learn of the outcomes of my patients. I worry that I might become overly sensitive to subtle ECG changes.
I'm glad you posted some false positive ECGs at the end of this post, however I don't fully understand why some are false positives. Especially case #3.
It would be great to see more of this in future posts.
Thanks
The ECGs are explained at all the links
DeleteThanks so much for these examples!!!
ReplyDeleteYou are welcome!
Deletei shall say this... i have a heck of whole lot more studying to do.
ReplyDeleteyes, after you, Steve and Ken, point out the 200 reasons it should be obvious to me, a simple ER doc, to activate the cath lab, which in my shop means either chopper to modesto, or stat ambulance lights and sirens to turlock, at the end of it all, i look again at the ECG at the very top of the blog, ECG #1 from triage , which has been placed in front of my face while i am writing orders on Cerner for three other patients, i simply can see that i need to do a whole heck of lot more studying , here and elsewhere, to not miss these. or to over-react, mis-react, on a normal variant.
but thank you both for these excellent, detailed attempts to teach me. and us.
tom
So much is just seeing examples over and over, for pattern recognition
Delete