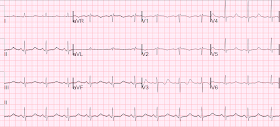
An alcoholic presented with confusion. He had this ECG recorded:
V3 reminds me of this ECG:
 |
| What do you think? Computer measures the QT at 505 ms, and QTc at 533 ms The measure appears to be correct. |
V3 reminds me of this ECG:
Are These Wellens' Waves??
These waves which you think are T-wave are really very large U-waves.
The clues are:
1) the down-up morphology
2) the apparent very long QT
The K returned at 2.1 ng/mL.
The pH was 7.55 and bicarb was 47, with chloride less than 68. The patient has a severe hypokalemic metabolic alkalosis from vomiting.
(By the way, the pCO2 was 55. An appropriate compensation for metabolic alkalosis is 0.9 x bicarb + 15. So 47 x 0.9 = 43. Add 15 and you get an expected pCO2 of 58. A pCO2 of 55 is just a bit below predicted.)
The importance of this is:
Anything that increases ventilation (hypoxia, agitation, anxiety) can lead to dangerous alkalemia.
If the pCO2 were to be lowered to normal (= 40), then the pH would rise to 7.70 (very dangerous).
Here are subsequent ECGs:
This one at K = 2.4
And 6 hours later at K = 2.6 mEq/L:
 |
| Now the apparent T-waves are really T-waves (not U-waves), and the QT is 479, QTc 500 |
Learning Points:
1. When the QT interval is impossibly long, the "T-waves" are probably U-waves. In this case, the QT was long, but not impossibly so. Nevertheless, one should think of U-waves.
2. When there are down up T-waves, and the apparent QT is long, they are probably U-waves.
3. Large U-waves are associated with a high risk of VT. (I will write more on this later)


Dear Dr Smith:
ReplyDeleteFirst of all thanks for your kindly knowledge transmission on this and all issues
I wish you would have been my professor in faculty
One point I would like to comment but I am not sure if it's of some value or useful clue.
In a aVR I see a bimodal repolarization but if you look carefully you can detect a K 2.4 ecg the end of T wave an the beggining of U(T wave descends before U goes below the isoelectric level. Could it be a key too? Thanks Joseph
Yes, good observation
DeleteFascinating ST-T-U waves. Nice that there are 3 serial tracings — but the last ECG still corresponded to a very low serum K+ = 2.6 mEq/L — so we really do not know what this patient’s ECG would look like if serum K+ (and presumably also serum Mg++) were corrected back to normal — nor do we know what this patient’s baseline ECG looked like prior to developing this severe electrolyte abnormality. Unfortunately, this makes it difficult to sort out what is “U” vs “T” vs “fused T + U”. Further correction of serum K+ with repeat ECG would probably add clarity as to what might still be “fused T + U” in this 3rd ECG. Great Learning Points by Dr. Smith! I’d add #4) In the presence of a long QTc (or long QU) interval — think: i) Drugs; ii) Lytes; iii) CNS catastrophe; and/or some combination of these. In an alcoholic with confusion — in addition to electrolyte disorders (low K+/low Mg++) — a CNS cause of the patient’s confusion (in addition to the alcohol) becomes important to consider. NICE case — THANKS for presenting!
ReplyDeleteThe K level was still below normal after 6 h observation. There was a problem with potassium supplementation to the patient?
ReplyDeletePiotr, sorry I do not know.
DeleteSteve
I’m not sure if Dr. Smith agrees with my views on this subject … I have always believed that low Mg++ is very commonly seen when there is low K++ (and vice versa) — and that both clinical as well as ECG effects of hypomagnesemia and hypokalemia are similar. Moreover, it is often very difficult to completely correct body stores of K+ unless and until serum Mg++ is corrected. We lack details in this case — We don’t know how K+ replacement was accomplished, nor how rapidly, nor what serum Mg++ levels were (nor whether if low these were corrected). Keeping in mind that >>95% of body stores of both cations are intracellular — it is important to remember that the serum level (ie, extracellular cation) is only a fraction of total body stores — such that relatively low (albeit still “within the laboratory range of normal) levels of either cation might not necessarily reflect adequate body stores. Bottom Line — We just don’t know enough to know the answer to the valid question you raise. Those questions often can only be answered after full treatment is completed (which may be long after the ED visit … ).
ReplyDelete