The case below was contributed by Pendell Meyers, an EM G1 at Mt. Sinai (the case did not come from Mt. Sinai though!)
Pendell is the lead author on our Modified Sgarbossa Criteria Validation Study.
Meyers HP. Limkakeng AT. Jaffa EJ. Patel A. Theiling BJ. Rezaie SR. Stewart T. Zhuang C. Pera VK. Smith SW. Validation of the Modified Sgarbossa Rule for Diagnosis of STEMI in the Presence of Left Bundle Branch Block. American Heart Journal 170(6):1255-1264; December 2015.
Before the case, a few comments:
Pendell and I just published a case report of a patient with left bundle branch block who presented with chest pain that then resolved. His ED ECG showed his baseline LBBB, with no evidence of MI. Over the ensuing hours, he developed classic T-wave inversion of Wellens' syndrome, but in the context of LBBB! Troponins were then positive, and the angiogram revealed a 99% LAD lesion with thrombus. The case demonstrates that Wellens' syndrome can occur in the context of LBBB.
Here is a link to the case report:
Today's case shows how, even in the context of LBBB, reperfusion of the inferior and lateral walls, just as with the anterior wall, can result in typical reperfusion T-waves (which is what Wellens' waves represent).
Wellens' syndrome represents a post (spontaneous) reperfusion state. This is why the patient is always pain free. The ST elevation is implied but was never recorded because the patient did not have an ECG during pain.
This is worth a look (7 serial ECGs showing evolution of Wellens' over time):
Case
An 82 year old had the acute onset of chest pain. Here is his first ECG, time zero:
The cath lab should have been activated at this point, but apparently it was not. Instead, another ECG was recorded at time 46 minutes:
The cath lab was activated and a circumflex occlusion was opened and stented, with a door to balloon time of 3 hours.
Here is the first ECG recorded after reperfusion:
Here is our formal study of posterior reperfusion T-waves, written by me and lead author Brian E. Driver (Hennepin) and published in Emergency Medicine Journal:
Here is a still later ECG after reperfusion:
Peak troponin T was 3.71 ng/mL, which is indicative of a large MI (Troponin T peaks are far lower than troponin I). Earlier recognition of the concordant ST elevation could have saved more myocardium.
With reperfusion, T-wave inversion even occurs in LBBB:
As an explorative substudy of our validation of the modified Sgarbossa criteria, Pendell and I and others studied T-wave inversion. We looked at serial ECGs on patients with acute coronary occlusion ACO) who underwent reperfusion and compared to serial ECG on patients without ACO. Unfortunately, as a result of our multisite study in which ACO came from many institutions and controls from one institution, only 6 of 45 patients with ACO and reperfusion had serial ECGs available, and all 245 patients without ACO had serial ECGs available.
Another very illustrative case:
Pendell is the lead author on our Modified Sgarbossa Criteria Validation Study.
Meyers HP. Limkakeng AT. Jaffa EJ. Patel A. Theiling BJ. Rezaie SR. Stewart T. Zhuang C. Pera VK. Smith SW. Validation of the Modified Sgarbossa Rule for Diagnosis of STEMI in the Presence of Left Bundle Branch Block. American Heart Journal 170(6):1255-1264; December 2015.
Before the case, a few comments:
Pendell and I just published a case report of a patient with left bundle branch block who presented with chest pain that then resolved. His ED ECG showed his baseline LBBB, with no evidence of MI. Over the ensuing hours, he developed classic T-wave inversion of Wellens' syndrome, but in the context of LBBB! Troponins were then positive, and the angiogram revealed a 99% LAD lesion with thrombus. The case demonstrates that Wellens' syndrome can occur in the context of LBBB.
Here is a link to the case report:
Dynamic T-wave inversions in the setting of left bundle branch block
Though Wellens' syndrome was described in the LAD territory, I have shown cases demonstrating that it occurs in any coronary distribution. That is to say, that reperfusion results in terminal T-wave inversion even if the involved territory is the inferior or the lateral wall.Today's case shows how, even in the context of LBBB, reperfusion of the inferior and lateral walls, just as with the anterior wall, can result in typical reperfusion T-waves (which is what Wellens' waves represent).
Wellens' syndrome represents a post (spontaneous) reperfusion state. This is why the patient is always pain free. The ST elevation is implied but was never recorded because the patient did not have an ECG during pain.
This is worth a look (7 serial ECGs showing evolution of Wellens' over time):
Classic Evolution of Wellens' T-waves over 26 hours
Case
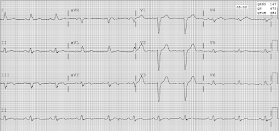
An 82 year old had the acute onset of chest pain. Here is his first ECG, time zero:
The cath lab should have been activated at this point, but apparently it was not. Instead, another ECG was recorded at time 46 minutes:
The cath lab was activated and a circumflex occlusion was opened and stented, with a door to balloon time of 3 hours.
Here is the first ECG recorded after reperfusion:
2 Examples of Posterior Reperfusion T-waves
(these are in the context of normal conduction, not LBBB)Here is our formal study of posterior reperfusion T-waves, written by me and lead author Brian E. Driver (Hennepin) and published in Emergency Medicine Journal:
Posterior reperfusion T-waves: Wellens' syndrome of the posterior wall
Here is a still later ECG after reperfusion:
 |
| There is evolution of T-wave inversion (deeper) in the affected leads. This is analogous "Wellens' waves" of the inferior and lateral leads, in the presence of LBBB! |
Peak troponin T was 3.71 ng/mL, which is indicative of a large MI (Troponin T peaks are far lower than troponin I). Earlier recognition of the concordant ST elevation could have saved more myocardium.
With reperfusion, T-wave inversion even occurs in LBBB:
As an explorative substudy of our validation of the modified Sgarbossa criteria, Pendell and I and others studied T-wave inversion. We looked at serial ECGs on patients with acute coronary occlusion ACO) who underwent reperfusion and compared to serial ECG on patients without ACO. Unfortunately, as a result of our multisite study in which ACO came from many institutions and controls from one institution, only 6 of 45 patients with ACO and reperfusion had serial ECGs available, and all 245 patients without ACO had serial ECGs available.
When this pattern was retrospectively defined as being either 1) present in at least two
contiguous anterior or inferior leads in at least two consecutive ECGs prior to reversal or 2) deeper than 3 mm in two contiguous leads (requiring only one ECG), it was found to be predictive of reperfused ACO (either spontaneously prior to catheterization or with mechanical reperfusion) with derived sensitivity and specificity of 5 of 6 [83% (95% CI 36–99%)] and 241 of 245 [98% (95% CI 96–99%)].
Meyers HP et al. Evaluation of T-Wave Morphology in Patients With Left Bundle Branch Block and Suspected Acute Coronary Syndrome
Another very illustrative case:
Here is a case of transient LAD occlusion that resulted in transient LBBB. After reperfusion, Wellens' waves are evident:



Regardless of whether one calls the changes we see here (in serial tracings on this case submitted by Wendell Meyers) as “Wellens Syndrome” in another coronary distribution — or simply evolutionary changes diagnostic of coronary occlusion followed by spontaneous reperfusion — the points to emphasize are: i) The sensitivity of the ECG for picking up acute evolving ST-T wave changes is reduced when there is a preexisting conduction defect; ii) That said, despite QRS widening on the baseline tracing (from LBBB or other conduction defect) — one CAN sometimes identify clear evidence of acute coronary occlusion in progress on the initial ECG (as was evident on the initial = Time Zero ECG in this case); iii) Serial ECG assessment can sometimes prove invaluable for removing any shadow of doubt that despite baseline QRS widening, acute STEMI is in progress. In this case, despite baseline LBBB — the ST-T waves we see in lead V6 on the initial tracing in the context of new chest pain are clearly abnormal — because with typical LBBB or RBBB, ST-T waves should normally be OPPOSITE to the last QRS deflection at least in leads I, V1 and V6. They are not in lead V6 here. And, in light of the definitely abnormal upright T wave in lead V6 on this initial ECG — the upright T wave in neighboring lead V5 is clearly taller-than-expected and abnormal. In a patient with new chest pain, regardless of the minimal amount of ST deviation in these leads — these ECG findings are diagnostic. And, in the 2nd ECG — lead-by-lead serial comparison should remove any doubts that might have remained, because of subtle-but-real increased amount of ST elevation now in leads II, III, aVF; V5 and V6 — in association with more reciprocal ST depression now in lead aVL. THANKS for presenting this GREAT case with important messages on assessing the ECG in a patient with new chest pain and baseline QRS widening.
ReplyDeleteThanks, Ken!
DeleteGreat Case & ECGs. I would also say that in addition to the disproportionate ST-Elevation in the inferior and lateral leads, even more salient are the classic hyperacute T-waves (the disparity after reperfusion is vast). Also interesting, in addition to the Posterior Reperfusion T-waves (although not meeting "Sgarbossa threshold" of 1mm) there appears to be "relative ST-depression" in V2 + V3 when the artery is occluded. Some really interesting findings. Incidentally, was this circumflex in a left-dominant heart?
ReplyDeleteThanks for sharing!
-SG
Sam,
DeleteAs above, circumflex!
Steve
Very instructive case demonstating that LBBB does not prevent us to diagnose not only STEMI but now even Wellens' pattern. Many thanks for presenting this case!
ReplyDeleteGlad you liked it, Mario!
DeleteSteve