This was sent to me, asking what I thought of it:
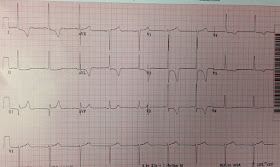
A very elderly woman presented with weakness and diarrhea. There was no chest pain or dyspnea.
An ECG was recorded because weakness is a common symptom of MI, especially in elderly women.
I was told the computer interpretation was "Acute STEMI".
My response was: "LVH only. No STEMI."
How do I know?
It is hard for me to explain exactly how I know this except that I have seen it so often and recognize the pattern. But I'll try.
Features suggesting STEMI:
One could easily believe this is inferior-posterior STEMI, as there is ST elevation in lead III with reciprocal ST depression in aVL, and there is ST depression in V2 and V3 with a tall R-wave (the mirror image of a posterior Q-wave).
However:
1. There is high voltage, especially in I, V2, and V3. aVL meets "criteria" for LVH of 11-12 mm amplitude. (As with most ECG features, however, morphology is more important than criteria)
2. The T-wave inversion might be mistaken for NonSTEMI, but then the locations are contradictory: The "inferior" ST elevation would imply active coronary occlusion of the inferior wall, while the T-wave inversion would suggest anterolateral NonSTEMI with reperfusion.
3. The ST elevation in III is not accompanied by any STE in II or aVF. In fact, II has some ST depression. This means that, in the frontal plane, the ST vector is directly to the right at 180 degrees. (In the axial plane it is also posterior, resulting in anterior ST depression)
4. ST elevation in III is a scooped-out saddleback, and that is because the ST segment is long and flat, and thus the T-wave is not hyperacute; rather, it has a narrow base. Contrast it with this wide-based T-wave in a true inferior STEMI:
[Although I have found that precordial ST elevation associated with Saddleback is almost never due to MI, I have not assessed it in inferior leads and am not sure of its significance.]
But doesn't all ST elevation with reciprocal ST depression in aVL mean Acute MI?
No! Absence of ST depression in aVL all but rules out pericarditis and early repolarization as the etiologies of inferior ST elevation. But reciprocal ST depression in aVL is frequently found in these STEMI mimics: LVH, LBBB, inferior LV aneurysm, myocarditis.
Much of ECG interpretation depends on pattern recognition
It is up to those of us who recognize the patterns to figure out what it is that we are seeing so we can communicate it to those who don't recognize it.
I have long thought that reading ECGs is like recognizing faces (maybe I'm autistic). I have long thought that we need to use computer facial recognition software that can learn from its mistakes, and train it to recognize these patterns.
Fortunately, I have come into contact with some software geniuses who know how to do this and we're hoping to improve ECG algorithms and make them self-teaching.
The patient did not have an MI.
A very elderly woman presented with weakness and diarrhea. There was no chest pain or dyspnea.
An ECG was recorded because weakness is a common symptom of MI, especially in elderly women.
 |
| What is your interpretation? |
I was told the computer interpretation was "Acute STEMI".
My response was: "LVH only. No STEMI."
How do I know?
It is hard for me to explain exactly how I know this except that I have seen it so often and recognize the pattern. But I'll try.
Features suggesting STEMI:
One could easily believe this is inferior-posterior STEMI, as there is ST elevation in lead III with reciprocal ST depression in aVL, and there is ST depression in V2 and V3 with a tall R-wave (the mirror image of a posterior Q-wave).
However:
1. There is high voltage, especially in I, V2, and V3. aVL meets "criteria" for LVH of 11-12 mm amplitude. (As with most ECG features, however, morphology is more important than criteria)
2. The T-wave inversion might be mistaken for NonSTEMI, but then the locations are contradictory: The "inferior" ST elevation would imply active coronary occlusion of the inferior wall, while the T-wave inversion would suggest anterolateral NonSTEMI with reperfusion.
3. The ST elevation in III is not accompanied by any STE in II or aVF. In fact, II has some ST depression. This means that, in the frontal plane, the ST vector is directly to the right at 180 degrees. (In the axial plane it is also posterior, resulting in anterior ST depression)
4. ST elevation in III is a scooped-out saddleback, and that is because the ST segment is long and flat, and thus the T-wave is not hyperacute; rather, it has a narrow base. Contrast it with this wide-based T-wave in a true inferior STEMI:
 |
| Lead III This is STEMI. There is no true saddleback because the T-wave is wide-based (it is particularly fat and bulky resulting in an absence of upward concavity). |
[Although I have found that precordial ST elevation associated with Saddleback is almost never due to MI, I have not assessed it in inferior leads and am not sure of its significance.]
But doesn't all ST elevation with reciprocal ST depression in aVL mean Acute MI?
No! Absence of ST depression in aVL all but rules out pericarditis and early repolarization as the etiologies of inferior ST elevation. But reciprocal ST depression in aVL is frequently found in these STEMI mimics: LVH, LBBB, inferior LV aneurysm, myocarditis.
Much of ECG interpretation depends on pattern recognition
It is up to those of us who recognize the patterns to figure out what it is that we are seeing so we can communicate it to those who don't recognize it.
I have long thought that reading ECGs is like recognizing faces (maybe I'm autistic). I have long thought that we need to use computer facial recognition software that can learn from its mistakes, and train it to recognize these patterns.
Fortunately, I have come into contact with some software geniuses who know how to do this and we're hoping to improve ECG algorithms and make them self-teaching.
The patient did not have an MI.

Great stuff Dr. Smith, really enjoyed that breakdown.
ReplyDeleteThanks!
DeleteHi Dr Smith,
ReplyDeleteCould I know any article that talks about the utility of St vector in MI? Coudl you share to me if there is any?
Thanks
Ryan
Ryan,
DeleteI searched google for it and my own article came up:
http://hqmeded-ecg.blogspot.com/2012/02/five-primary-patterns-of-ischemic-st.html
Another good one: http://www.medscape.com/viewarticle/545741_1
Vince De Guglio has take my thoughts in more depth: http://www.ems12lead.com/2014/05/08/conclusion-to-masters-case-01/
Steve
My initial concern was that the T-wave inversions in V2-3 would represent hyperacute T-waves of the posterior wall. Is there a way to differentiate that from reperfusion T-waves?
ReplyDeleteMagnus
Magnus,
DeleteThey are just too deep to be from posterior MI. But very typical of LVH.
STeve
Very common pattern of LVH......I dont know the reason but isolated STE in L3 is very common denominator in this scenario . Secondly,a common ECG basic should not be forgotten....very large voltage always screws up the preceeding T wave @ Amal Mattu.
ReplyDeleteYes, always. I have said this in many many posts!
DeleteDr. Arora...
DeleteIf you look at aVL you'll see why there is often a bit of ST elevation in Lead III with LVH. The positive poles of Lead III and aVL are almost opposite each other. In LVH, Lead aVL - being left-sided - will often show a repolarization abnormality. And remember that Lead III = aVF - aVL. Many of the older texts will state the ST-T changes of a repolarization abnormality start at the baseline but in actuality they usually do NOT. There is almost always some ST segment deviation at the J point. In the ECG that Steve has presented, look at aVL: it has a repolarization abnormality that begins below the J point. Lead aVF won't change anything here because its ST segment is not deviated (ie, it's neutral). Thus, the "STE" in Lead III is really just reflecting the slight ST depression in aVL due to the repolarization abnormality.
Jerry W. Jones, MD FACEP FAAEM
Steve...
ReplyDeleteHow would you explain the large R wave voltage in V2 and V3 which are right-sided leads? Also, the T wave inversion in V3 is definitely not due to repolarization abnormality. Look at the plateau between the J point and the beginning of the T wave in V3. Although the beginning of a repolarization abnormality may deviate positively or negatively from the J point, it nonetheless still begins at the J point. There should be no baseline delay between the QRS and the T wave. One could make the same argument for V2 here also, though admittedly it is not quite so clear. There is obviously some counterclockwise rotation also. The forces in V2 and V3 are very anterior. I'm wondering if there might not be a bit of apical hypertrophic cardiomyopathy here. The septum actually forms a good bit of the "anterior wall" of the left ventricle since the septum is actually almost parallel to the frontal plane and the true anterior wall is actually rotated a bit superiorly.
Jerry W. Jones MD FACEP FAAEM
Jerry,
DeleteV2 and V3 are not right sided leads. They are left sided and represent anterior hypertrophy, without the typical leftward rotation that is normally seen in LVH. HOCM is possible, or even likely, I do not know.
Steve
Clinically, however, I'll go for serial trop & enzymes, if the ECG changes are new and no convincing explanation for her symptoms.
ReplyDeleteThat is of no help in deciding whether to activate the cath lab. None whatsoever!!
DeleteSteve,
ReplyDeleteLove your description of how we recognize patterns and may not even be able to fully explain without thinking hard about it why we know what we are seeing. It reminds of when we walk out of a patient room and we have an impression and we may not be able to put our finger on why we have that impression (something they said, something in their tone, a facial expression, etc). I agree with all your observations on why this just does *not* look like inferior STEMI, but one the most glaring missing puzzle piece for me is the quiet t-wave in Lead II. I could be convinced the t-waves in III & aVF are hyperacute, but you just don't see this with that tiny T-wave in Lead II!
Sam
Good observation, Sam!
Delete