A male is his 30's with h/o HTN presented after 6 hours of chest pain. The pain was crushing and substernal, associated with nausea, vomiting, and diaphoresis, radiating to his back, 10 out of 10 in intensity, the "worst pains ever experienced". He described the sensation as "an elephant sitting on chest". Here is his EKG by EMS:
The cath lab was activated prehospital. Patient received 324 aspirin and 3 nitroglycerin tablets sublingually prior to arrival to the ED with mild improvement of pain.
Here is the ED ECG:
Suppose you were at a small hospital that only has thrombolytics. You have the option of giving thrombolytics or of transferring to a PCI capable hospital. The Door (small hospital) to Balloon (PCI hospital) time will be 90 minutes.
Should you give thrombolytics?
It is well known that thrombolytics work best with fresh thrombus, within 2 hours of onset of occlusion (Steg et al., see reference 8 below). But this patient has had 5 hours of chest pain.
However, the ECG shows a very high level of "Acuteness," as demonstrated by 1) the size of the T-wave 2) the amount of ST elevation and 3) the absence of Q-waves. Hyperacute T-waves are present when there is a large amount of viable, salvageable, myocardium. As the myocardium infarcts (Q-waves), rather than being "injured," (as manifested by ST elevation and hyperacute T-waves), the size of the T-wave diminishes, and also the ST elevation diminishes and Q-waves begin to form (although in anterior STEMI Q-waves may form very early due to ischemia of the conducting system, not infarct!).
The most specific sign of a very early MI are hyperacute T-waves.
We know that ACS is a very dynamic process, with opening and closing of the vessel. The time of onset of chest pain is not a good determinant of the time of onset of irreversible ischemia (infarct). We also know that pain is not a very reliable indicator of reperfusion/reocclusion. Studies of patients on 12-lead ST segment monitors shows rise and fall of ST segments while patients are asymptomatic.
So, this ECG is very hyperacute. Almost all the myocardium at risk is viable and can be salvaged. The thrombus has been forming and lysing spontaneously, which means that it is fresh thrombus, and very amenable to lysing with tPA or TNK-tPA.
If I saw this patient, assuming there are no contraindications, I would give thrombolytics (fibrinolytics) and transfer.
When the patient arrives at the PCI-capabel hospital, if there is no reperfusion, as measured by less than 50% ST-segment resolution in the single lead with maximum elevation, or clinical evidence of failed reperfusion within 90 minutes after fibrinolysis, then rescue coronary intervention can be performed. See this article in the New England Journal.
Outcome
The patient went for angiogram/PCI, and a 100% mid-LAD occlusion was found and opened.
The peak troponin I was 0.9 ng/mL (very low). The ECG the next day is here:
Echocardiogram next day: There was a mild antero-apical wall motion abnormality. The convalescent echo, which is done after recovery of "stunned" myocardium at 4-6 weeks, will almost certainly be normal.
Of the significant myocardium at risk in the anterior wall, almost all of was salvaged because of the hyperacute nature of the injury, as manifested by huge T-waves, and the rapid reperfusion.
Lesson:
1. The ECG is a better indicator of acuteness than the time since onset of chest pain.
2. When the ECG is very acute, thrombolytics are beneficial, and waiting for PCI has much less benefit, and probably relative harm.
Relevant references, in addition to the New England Journal article above
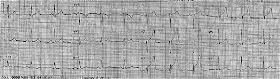 |
| Obvious anterior STEMI with very large T-waves. Is this consistent with 5 hours of injury? |
The cath lab was activated prehospital. Patient received 324 aspirin and 3 nitroglycerin tablets sublingually prior to arrival to the ED with mild improvement of pain.
Here is the ED ECG:
 |
| Very hyperacute T-waves and ST elevation. Somewhat diminished after Nitroglycerine. |
Suppose you were at a small hospital that only has thrombolytics. You have the option of giving thrombolytics or of transferring to a PCI capable hospital. The Door (small hospital) to Balloon (PCI hospital) time will be 90 minutes.
Should you give thrombolytics?
It is well known that thrombolytics work best with fresh thrombus, within 2 hours of onset of occlusion (Steg et al., see reference 8 below). But this patient has had 5 hours of chest pain.
However, the ECG shows a very high level of "Acuteness," as demonstrated by 1) the size of the T-wave 2) the amount of ST elevation and 3) the absence of Q-waves. Hyperacute T-waves are present when there is a large amount of viable, salvageable, myocardium. As the myocardium infarcts (Q-waves), rather than being "injured," (as manifested by ST elevation and hyperacute T-waves), the size of the T-wave diminishes, and also the ST elevation diminishes and Q-waves begin to form (although in anterior STEMI Q-waves may form very early due to ischemia of the conducting system, not infarct!).
The most specific sign of a very early MI are hyperacute T-waves.
We know that ACS is a very dynamic process, with opening and closing of the vessel. The time of onset of chest pain is not a good determinant of the time of onset of irreversible ischemia (infarct). We also know that pain is not a very reliable indicator of reperfusion/reocclusion. Studies of patients on 12-lead ST segment monitors shows rise and fall of ST segments while patients are asymptomatic.
So, this ECG is very hyperacute. Almost all the myocardium at risk is viable and can be salvaged. The thrombus has been forming and lysing spontaneously, which means that it is fresh thrombus, and very amenable to lysing with tPA or TNK-tPA.
If I saw this patient, assuming there are no contraindications, I would give thrombolytics (fibrinolytics) and transfer.
When the patient arrives at the PCI-capabel hospital, if there is no reperfusion, as measured by less than 50% ST-segment resolution in the single lead with maximum elevation, or clinical evidence of failed reperfusion within 90 minutes after fibrinolysis, then rescue coronary intervention can be performed. See this article in the New England Journal.
Outcome
The patient went for angiogram/PCI, and a 100% mid-LAD occlusion was found and opened.
The peak troponin I was 0.9 ng/mL (very low). The ECG the next day is here:
Echocardiogram next day: There was a mild antero-apical wall motion abnormality. The convalescent echo, which is done after recovery of "stunned" myocardium at 4-6 weeks, will almost certainly be normal.
Of the significant myocardium at risk in the anterior wall, almost all of was salvaged because of the hyperacute nature of the injury, as manifested by huge T-waves, and the rapid reperfusion.
Lesson:
1. The ECG is a better indicator of acuteness than the time since onset of chest pain.
2. When the ECG is very acute, thrombolytics are beneficial, and waiting for PCI has much less benefit, and probably relative harm.
Relevant references, in addition to the New England Journal article above
1. Engblom H, Strauss DG, Heden B, et
al. The evaluation of an electrocardiographic myocardial ischemia acuteness
score to predict the amount of myocardial salvage achieved by early
percutaneous coronary intervention Clinical validation with myocardial perfusion
single photon emission computed tomography and cardiac magnetic resonance. J
Electrocardiol 2011;44(5):525-32.
2. Armstrong PW, Fu Y, Westerhout CM,
et al. Baseline Q-wave surpasses time from symptom onset as a prognostic marker
in ST-segment elevation myocardial infarction patients treated with primary
percutaneous coronary intervention. J Am Coll Cardiol 2009;53(17):1503-9.
3. Sejersten M, Ripa RS, Maynard C, et
al. Timing of ischemic onset estimated from the electrocardiogram is better
than historical timing for predicting outcome after reperfusion therapy for
acute anterior myocardial infarction: a DANish trial in Acute Myocardial
Infarction 2 (DANAMI-2) substudy. Am Heart J 2007;154(1):61 e1-8.
4. Engblom H, Heden B, Hedstrom E,
Wagner G, Arheden H. ECG Estimate Of Ischemic Acuteness and Time from Pain
Onset for Predicting Myocardial Salvage in Patients Undergoing Primary
Percutaneous Coronary Intervention. AHA Abstract 2404. Circulation
2007;116(Suppl II):II_528.
5. Wong CK, Gao W, Raffel OC, et al.
Initial Q waves accompanying ST-segment elevation at presentation of acute
myocardial infarction and 30-day mortality in patients given streptokinase
therapy: an analysis from HERO-2. Lancet 2006;367:2061-7.
6. Gersh BJ, Stone GW, White HD, Holmes
DR, Jr. Pharmacological facilitation of primary percutaneous coronary
intervention for acute myocardial infarction: is the slope of the curve the
shape of the future? JAMA 2005;293(8):979-86.
7. Taher T, et al. Aborted myocardial
infarction in patient with ST segment elevation: Insights from the Assessment
of the Safety and Efficacy of a New Thrombolytic Regimen-3 Trial
Electrocardiographic Substudy. J Am Coll Card 2004;44:38-43.
8. Steg PG, Bonnefoy E, Chabaud S, et
al. Impact of time to treatment on mortality after prehospital fibrinolysis or
primary angioplasty: data from the CAPTIM randomized clinical trial.
Circulation 2003;108(23):2851-6.
9. Heden B, Ripa R, Persson E, et al. A
modified Anderson-Wilkins electrocardiographic acuteness score for anterior or inferior
myocardial infarction. Am Heart J 2003;146(5):797-803.
10. Corey KE, Maynard C, Pahlm O, et al.
Combined historical and electrocardiographic timing of acute anterior and
inferior myocardial infarcts for prediction of reperfusion achievable size limitation.
Am J Cardiol 1999;83(6):826-31.
11. Hochrein J, Sun F, Pieper KS, et al.
Higher T-wave amplitude associated with better prognosis in patients receiving
thrombolytic therapy for acute myocardial infarction (a GUSTO-1 substudy). Global Utilization of Streptokinase and
Tissue plasminogen activator for Occluded Coronary Arteries. Am J Cardiol
1998;81(9):1078-84.
12. Wilkins ML, Pryor AD, Maynard C, et al.
An electrocardiographic acuteness score for quantifying the timing of a
myocardial infarction to guide decisions regarding reperfusion therapy. Am J
Cardiol 1995;75(8):617-20.
13. Anderson ST, Wilkins M, Weaver WD,
Selvester RH, Wagner GS. Electrocardiographic phasing of acute myocardial
infarction. J Electrocardiol 1992;25 Suppl:3-5.


Interesting that there are no inferior or lateral/AVL reciprocal changes?
ReplyDeleteThere is a bit of STE in V5, and an inverted T-wave in III. But anterior STEMI due to mid LAD occlusion frequently has no reciprocal changes. It is a common misconception that they always do.
DeleteCorrection I do see very small lateral changes
ReplyDeleteThanks Dr.Smith.. although I kept in mind other DDX like HyperK, the pain is worrisome to consider thrombolytics
ReplyDeletethe shape of ST is concave up . the ST is > 3mm in v2-v3...
although defines criteria for MI, but in most of the time i have seen such ECG warrants more confirmatory studies like serial ECGs and ECHO.. probably due to fear of TPA
There is simply too much ST elevation and too large a T-wave for this to be anything but STEMI. If you apply my STEMI vs. early repol equation: QTc was 410 ms, STE at 60 ms after the J-point in lead V3 = 5 mm, and R-wave amplitude in V4 = 20 mm, the result is 23.6 which is (barely) > 23.4. Also, the preshospital ECG has even more ST elevation, so there is some decrease associated with the improvement of pain with NTG. You can always quickly measure the K, although this does not look like hyperK. It was normal.
DeleteIn V3 and V4 there also seems to be some terminal QRS distortion, like the S wave is pulled up higher than it would normally be. Do you agree?
ReplyDeletePendell,
DeleteI do agree, and think it very much contributes to the diagnosis. however, it does not meet Birnbaum's criteria (not that that matters):
QRS Distortion is defined as: "Emergence of the J point ≥50% of the R wave in leads with qR configuration, or disappearance of the S wave in leads with an Rs configuration)" (from this paper by Birnbaum). I would add to this: if there are distinct J-waves in these leads, then early repolarization is still a likely possibility. In this case, there are no distinct J-waves in V2 or V3 (although there is a small one in V4)
Steve
Ecg after pci shows Wellen's t wave, in literature Wellen's t wave suggest that it's
ReplyDeletetight narrowing of lad
In this case after pci Wellen's t wave developed it means pci failed or new obstruction occur-if I wrong pz correct me
No. Wellens' T-waves are always AFTER an episode of pain, and when no ECG was recorded DURING the pain. But we know from reperfusion trials that this is exactly the same kind of T-wave inversion we get after reperfusion. So, extrapolating backward in time, those who have Wellens' had upright T-waves with ST elevation at the time of their pain. They had spontaneous reperfusion (which is very common in STEMI) and when the were pain free with open artery (or good collateral circulation), then the ECG was recorded and showed T-wave inversion. In Wellens' study, all 180 patients had EITHER an open LAD or good collateral circulation to the anterior wall.
ReplyDelete