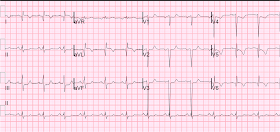
A man in his 50's complained of typical chest pain. Here is his ED ECG:
The patient had been ruled out by serial troponins at the previous hospitalization. He had not had an echocardiogram or any stress testing or angiogram. The etiology of the abnormal baseline ECG is uncertain. Is it due to a previous anterior MI? Very likely.
Because there was no significant change, the cath lab was not activated. Serial ECGs were recorded and showed no evolution. The patient ruled out for MI by serial troponins, but, again, did not have a stress test or echocardiogram.
Lesson:
1. Always check old ECGs, if available, when there is a subtle ECG with possible STEMI.
2. Serial ECGs can help to clarify the situation.
 |
| Nearly identical to the first. However, the first one has slight straightening of the ST segments in V2 and V3, which are suspicious. |
The patient had been ruled out by serial troponins at the previous hospitalization. He had not had an echocardiogram or any stress testing or angiogram. The etiology of the abnormal baseline ECG is uncertain. Is it due to a previous anterior MI? Very likely.
Because there was no significant change, the cath lab was not activated. Serial ECGs were recorded and showed no evolution. The patient ruled out for MI by serial troponins, but, again, did not have a stress test or echocardiogram.
Lesson:
1. Always check old ECGs, if available, when there is a subtle ECG with possible STEMI.
2. Serial ECGs can help to clarify the situation.