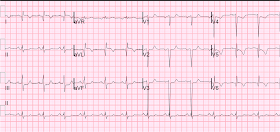
A middle aged male with h/o CAD presented with chest pain. He had a recent previous stent in the circumflex. Here is the ECG at time = 0:
Here is the previous ECG from one month prior:
Opiates in Acute Coronary Syndrome:
Opiates are associated with 1.5x mortality in ACS. Why? Probably because they lead the physician to a false sense of security. In this case, the absence of any further chest pain was reassuring to the physicians.
See this reference with full text link:
 |
| What do you think? |
Here is the previous ECG from one month prior:
 |
| Now what do you think? |
The first ECG shows Q-waves in lateral leads, and T-wave inversion as well, wit ST elevation in I and aVL. There is ST depression in V2-V5, 1 mm in V3, diagnostic of posterior STEMI. Thus, this is posterolateral STEMI. The Q-waves may lead one to believe that this is a subacute STEMI with a prolonged duration, long enough to result in infarction in addition to injury. But the pain duration was only 1 hour.
Comparison with the previous ECG confirms that this is acute STEMI superimposed on a previous lateral MI (old lateral Q-waves, old T-wave inversions). The ST elevation in I and aVL is definitely new. And now it is clear that the ST depression in V2-V5 is very marked, as there is 3.5 to 4 mm of relative ST depression in V3.
It is not clear that the treating physicians saw the previous ECG. They were uncertain of the diagnosis and called an immediate cardiology consult. Hydromorphone relieved all the pain, which helped ease the anxiety of the physicians. The cardiologist arrived immediately, but did not immediately activate the cath lab. They ordered this repeat ECG at time = 51 minutes:
 |
| Now it is very clear that there is an acute posterior STEMI. |
An unusual feature of this case is the persistent negative T-waves in the affected leads. Normally, with occlusion of the infarct-related artery, negative T-waves from previous MI will become upright (pseudonormalization). So one would expect, if this is indeed STEMI, upright T-waves in I, aVL, V5 and V6.
An immediate echocardiogram was ordered which confirmed new posterolateral wall motion abnormality and old anterior and apical wall motion abnormality. The patient underwent PCI with stent of occluded proximal circumflex near the ostium of the first obtuse marginal where the previous stent had been placed. The maximum troponin I was 80 ng/ml.
Here is the post-PCI ECG:
 |
| Notice the tall and large precordial T-waves. These are what I call Posterior reperfusion T-waves. They are the analog of Wellens' T-waves and if recorded from the posterior wall would look like Wellens' T-waves. But because the leads are over the anterior wall, then they are large and upright, rather than inverted! |
Opiates in Acute Coronary Syndrome:
Opiates are associated with 1.5x mortality in ACS. Why? Probably because they lead the physician to a false sense of security. In this case, the absence of any further chest pain was reassuring to the physicians.
See this reference with full text link:

t=0 seems quite obvious. as i read this post i can't help but think of all the times physicians were dismissive of what i thought were significant ECGs.
ReplyDeleteYes. Sometimes even providers who are excellent at reading ECGs can miss things that seem obvious to others, and which at other times they would not miss.
ReplyDeleteThe cardiologists called it a NonSTEMI.
this pt had significant history and significant presentation. i wonder why that is when otherwise excellent clinicians miss something like this... fatigue, distractions, complacency, burnout, tunnel-vision?
ReplyDeleteas i look back i myself often wonder what i was thinking when i did all sorts of stupid things in retrospect.
Indeed, it is the things that cloud our minds which are the biggest obstacle to good medicine.
DeleteThe recent intervention to LCx raises the odds of this chest pain to be ischemic & it must be dealt with as a remark of stent thrombosis till proven otherwise. The inferior reciprocal ST depression that was present on the first EKG should alert the physician to the possibility to high lateral STEMI, in addition to the precordial ST depression in leads with baseline STE from previous infarction.
ReplyDeleteRegarding the the hyperacute T wave, I think you are 100% right as usual. I personally follow (2) cases in our cath. laboratory, one was with LCx procedure-related dissection that was stented successfully & the other was inferoposterior STEMI that underwent PPCI, both of them develop hyperacute T wave in the postop. period in the precordial leads (V1-V3) with complete resolution of the chest pain.
Such cases as I think will motivate us as physicians more & more to scrutinize EKGs in patients with chest pain.
Thank you, Ali.
DeleteThis comment has been removed by the author.
ReplyDeleteThank you Dr Smith great case as usual.
ReplyDeleteI wish to ask a question to clarify in my mind, you made the statement 1mm of ST depression in V2-5 is diagnostic of posterior AMI. This ECG time 0 has the lateral ST elevation to help in the diagnosis, but if this was a pure posterior AMI would you need to do posterior leads to truely make the diagnosis. I ask as I work in a centre that thrombolyses only (2-3hrs from a PCI centre) and limited access to emergency ECHO, is the depression enough to thrombolyse on.
Regards
Matt
Yes. It would be helpful to get posterior leads, but in this case you have not just posterior MI, but posterolateral MI. The ST depression is maximal in V2 and V3 (the relative depression is profound) and there is ST elevation in I and aVL, with reciprocal depression in III. So this is diagnostic and lytics are indicated. You should read my very popular post "Five Primary Patterns of ischemic ST depression" See sidebar under "popular posts".
Delete