Written by Magnus Nossen
The below ECG is from a 40 something male with no past relevant medical hx. The patient contacted EMS due to sudden onset chest pain, palpitations and lightheadedness. Symptoms occurred while playing soccer.
Upon seeing this ECG what is your initial interpretation? What is your next step in the management of this patient?
The initial ECG in todays case was recorded by EMS and shows a very rapid wide complex tachycardia with a heat rate @ about 245 bpm. This is a very fast arrhythmia and most adult patients even if healthy will likely show signs of hemodynamic compromise (hypotension, chest pain, dyspnea) at such fast heart rates if the arrhythmia persists. Cardioversion should be your next step in the management of this patient. The 12 lead ECG can be scrutinized later.
The patient was «tolerating» the arrhythmia initially (maintaining BP) and was given iv amiodarone by the paramedics en route to the hospital.
Upon arrival he was diaphoretic and profoundly hypotensive. (SBP in the 60s) Measures for immediate cardioversion were undertaken. While the patient was being administered propofol for sedation, the arrhythmia spontaneously terminated. No shock was delivered. The patient’s blood pressure and condition improved instantly.
Now it is time to have a closer look at the prehospital ECG. The tracing shows a wide complex tachycardia in which the QRS is completely negative in leads II, III and aVF. In the precordial leads there are QS waves in V1-V4. R/S transition occurs late, between lead V5 and V6. The QRS vector is positive in the lateral leads (I and aVL). The QRS axis is directed superiorly and laterally. In the precordial leads there is «LBBB-like» morphology. Together, the frontal plane axis and QRS morphology point toward origin of the arrhythmia from the apical portion of the right ventricle.
The initial ECG post conversion (not shown) revealed widespread ST-T wave changes as expected following a sustained very rapid tachycardia. Below is a repeat ECG acquired roughly 15 minutes after cessation of the tachyarrhythmia.
What do you think about the resting ECG? What abnormalities can you identify in this 12 lead?
Smith: The layout here is the Cabrera format, which uses a clockwise format from upper left (aVL) around to I, -aVR, II, aVF, and III.
The resting ECG is not normal for a 40 something male. The tracing shows atrial fibrillation which is very uncommon in a healthy 40 something old male. The QRS is narrow with slight q waves in an inferolateral distribution. Most striking are the pathologic T wave inversions in the precordial leads extending all the way to V6, and also in II, III, aVF (all these T-wave inversions are typical of RV cardiomyopathy).
You might ask if the T-wave inversion in the precordial leads could be related to the preceding tachycardia. Could they be memory T waves? Or maybe T inversions from demand ischemia? The T waves in the precordial leads simply do not look like memory T waves. Also, usually longer periods of abnormal depolarization is required for memory T wave phenomenon to occur. There was an old ECG on file with similar findings in the early precordial leads. This essentially rules out demand ischemia as a cause. (The old ECG was not recognized as pathologic at the time of recording). T wave inversions are more pronounced in the right precordial leads and there is no good reason for a tachydysrhythmia to give demand ischemia mostly in the RV in a presumably healthy individual.
There are PVCs with a distinctly different axis and morphology as compared to the wide complex tachycardia. (The PVCs in this tracing seem to have an RVOT morphology).
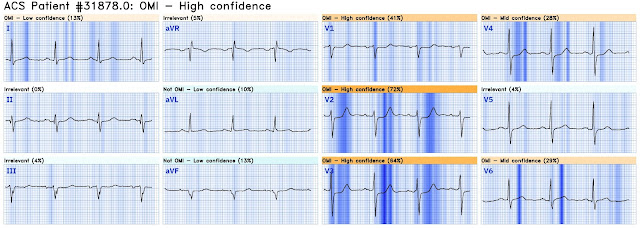
In summary the wide complex tachycardia and the resting ECG should alert you to right ventricular pathology. I put this ECG through the QoH for digitization purposes and the QoH AI algorithm was not fooled by the ST-T changes in this ECG. The interpretation was not OMI with high confidence.
From the available information, the following diagnoses could conceivably be on the list of differentials
- Arrhythmogenic (RV) cardiomyopathy with VT
- RV myocardial scar/ischemia causing VT
- Any myocardial disease affecting the RV (e.g. myocarditis/sarcoidosis etc)
- Antidromic AVRT with a right sided posterolateral AP
- Mahaim fibre mediated tachycardia
- RVOT, but RVOT should have an inferior axis, not a superior axis as in this ECG
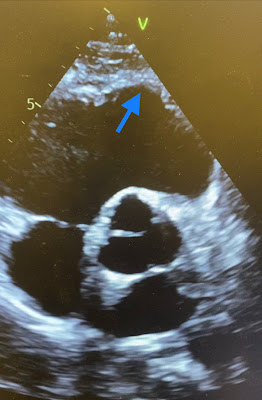
After the arrhythmia terminated the patient stabilized quickly and a bedside echocardiogram was obtained. The videos below show focused views of the right ventricle. The RV is dilated with decreased systolic performance, there is myocardial thinning and hypokinesis of the large areas of the RV, especially the apical regions and RVOT. RV EF on formal study was 34%. Right ventricular end diastolic volume (RVEDV) was significantly increased. Also noted was hypokinesis involving the LV in a non-coronary pattern. LVEF was preserved.
Below are focused views on the right ventricle (left frame) and RVOT (right frame). The videos show that both the RV and the outflow tract are significantly dilated. The RV myocardium shows regional myocardial thinning and aneurysms.
Below are still images with red arrows pointing to the dilated basal and apical regions of the RV. Circled in yellow is the midventricular region of the RV which shows less dilatation likely owing to restrain by the moderator band. Blue arrows point toward thinning of the myocardium both in the apical region of the RV and in the RVOT.
Discussion: Putting all of the information together this patient is most likely suffering from arrhythmogenic cardiomyopathy (AC) better known as ARVC. The medical hx is typical, with sudden onset tachydysrhythmia during physical exertion. It is not uncommon for the initial presentation to be sudden cardiac death (SCD). In fact it is one of the leading causes of SCD in people age less than 40 years. Thus it is very important to identify this disorder. AC is a disease in which myocardium is replaced by fibrofatty tissue. This usually and predominantly affects the RV free wall and apical regions, but it can affect the left ventricle as well and this is why arrhythmogenic cardiomyopathy is a more precise name for the disorder than ARVC.
Smith: The 5 entities I look for on all ECGs for patients with syncope who are asymptomatic on arrival with sinus rhythm and no ischemia is:
1. WPW
2. HOCM
3. Brugada
4. Long QT
5. RV cardiomyopathy
The origin of the VT in our case is from the apical portion of the RV. There are signs of RV pathology on the ECG (T wave inversions in V1-V3). I do not see any epsilon waves in the post conversion ECG. T wave inversion extends throughout the precordial leads all the way to V6 signifying involvement also of the left ventricular myocardium. This was consistent with echocardiographic and MRi findings in this case. Atrial fibrillation too has an association with ARVC.
Diagnosis of AC is based on the family hx, patient hx, electrocardiographic, echocardiographic and radiologic features as well as genetic studies. The diagnostic criteria are complex. Clinical and paraclinical findings are grouped into major and minor criteria. For a definite diagnosis 2 major criteria, 1 major and two minor or 4 minor criteria are required.
Some information on epsilon waves and late potentials: In ARVC late potentials are thought to be caused by early afterdepolarizations of cells in the (right) ventricle. Their amplitude is often too small to show up on a normal ECG. However, when multiple QRS recordings (typically > 200 consecutive QRS complexes) are averaged, random noise is filtered out and late potentials can show up. Such a recording is called a Signal Averaged ECG (SAECG).
Sometimes late potentials can manifest on the regular ECG as epsilon waves. Although the epsilon wave is considered a major diagnostic criterion for arrhythmogenic cardiomyopathy (AC) its diagnostic value is limited because it is a sign of the later stage of the disease. It would be more appropriate to say that the epsilon wave is a “hallmark” of AC, but is of low diagnostic sensitivity. Although the epsilon wave has high specificity for AC, it can be present in other pathological conditions.
As previously mentioned, epsilon waves are not present in the post conversion ECG. Several ECGs were recorded for the patient in today's case. A few days into the hospital stay the patient’s rhythm spontaneously converted to sinus. Another ECG was recorded. The precordial leads are shown below in 50mm/s. Perhaps there was a difference in filter setting but epsilon waves now seem to be readily appreciable in leads V1-V3.
As there are epsilon waves in this case (major criteria) a pathologic SAECG does not really add any diagnostic value. (See this link for a very good discussion on signal averaged ECG)
Patients with AC should be educated with regards to their condition. Strenuous exercise is not recommended as it is thought to lead to disease progression. Malignant arrhythmias in AC patients tend to occur during physical exertion. Antiarrhythmic treatment with betablocker is mainstay and ICD placement should be considered for all patients with syncope or documented ventricular arrhythmia. The patient in today's case was put on betablocker and was given an implantable cardioverter/defibrillator (ICD). Long term follow up is not available.
Learning points:
1) AC is not limited exclusively to the RV although RV involvement is the hallm
ark of the disease.
2) Physical exercise may hasten disease progression. Strenuous exercise should be avoided.
3) Epsilon waves are highly suggestive of arrhythmogenic cardiomyopathy, but they are not pathognomonic as they can occur in other disease states (e.g. sarcoidosis).
4) AC is a chronic progressive disease. Beta-blocker and ICD are used to reduce arrhythmia incidence and arrhythmia related SCD.
5) Sometimes VT ablation can be performed and in rare cases heart transplantation is required.
Please see below cases for more on arrhythmogenic cardiomyopathy.
===================================
MY Comment, by KEN GRAUER, MD (3/22/2024):
===================================
ARVD is not a common entity. It's estimated incidence in the general population is ~1 per 2,500-to-5,000 (Shah et al: StatPearls — 2023). However, among younger adults who die suddenly — ARVC/D (Arrhythmogenic Right Ventricular Cardiomyopathy-Dysplasia) may be the cause in up to 5-10% of cases (with this prevalence range depending on demographics and the geographic area of the group studied). - From the above statistic, it should be apparent that while ARVC/D is uncommon (if not rare) in the general population — it clearly is an important entity to consider when a younger adult presents for emergency care because of a malignant ventricular arrhythmia.
- Dr. Meyers' case in the June 3, 2023 post of Dr. Smith's ECG Blog illustrates how despite the infrequency of ARVD (ie, Dr. Meyers had not previously made this diagnosis de novo despite his extensive ED experience!) — Workup and recognition of ARVD as the cause of the patient's presenting VT episode in this June 3, 2023 case led to probable lifesaving implantation of an AICD in this previously healthy young woman.
Similarly, the previously healthy 40-something man presented by Dr. Nossen in today's case features yet another younger adult for whom recognition of ARVD as the cause of his VT episode — once again led to probable lifesaving ICD implantation.- With this as introduction — I add the following to Dr. Nossen's insightful presentation:
=====================================
Regarding the Initial ECG:
- The most common cause of sustained VT in a previously healthy younger adult — is idiopathic VT. As we've discussed on a number of occasions in Dr. Smith's ECG Blog (See My Comment and summarizing Table in Figure-2 of the February 14, 2022 post) — the Fascicular VTs and the Outflow Track VTs ( = RVOT VT and LVOT VT) are by far, the most common forms of idiopathic VT.
- Most of the time — the frontal plane axis and QRS morphology on ECG obtained during the VT episode allow ready recognition if one of the above common forms of idiopathic VT is the cause. On occasion, however — distinction between ARVD vs RVOT VT may not be possible on the basis of a single ECG, because both entities may manifest a LBBB-like pattern in the chest leads in association with an inferior axis in the frontal plane.
- In addition (as per Dr. Nossen) — given the expanded classification of "ARVD" based on the finding of not only RV, but also potential for LV involvement (ie, AC = Arrhythmogenic Cardiomyopathy) — the BOTTOM Line in 2024, is that ECG features are not sufficiently reliable to be depended on for identification of all cases of AC. As a result, in addition to Echo — virtually all younger adults who present with an episode of sustained VT should undergo Cardiac MRI to rule out a more severe form of underlying cardiac pathology.
- The above said, the initial ECG in today's case (that I have reproduced in Figure-1) does not resemble any of the common types of idiopathic VT because: i) There is marked QRS widening; ii) The shape of the QRS is amorphous (not resembling any known form of conduction defect); — and, iii) There is extreme axis deviation ( = an all negative QRS in each of the inferior leads). KEY Point: Echo and MRI are essential components for evaluation in today's case. This would be true regardless of whether epsilon waves are or are not seen on baseline or subsequent ECGs of the patient.
-USE.png) |
| Figure 1: The initial ECG in today's case. |
=====================================
Additional Thoughts on Epsilon Waves:
Since questions continually arise regarding the recognition of epsilon waves — I thought it useful to excerpt parts of my discussion from the above cited June 3, 2023 post in Dr. Smith's ECG Blog.
Why is it so difficult to pick up epsilon waves on a standard 12-lead ECG?
- There are several reasons ...
Reason #1: The Wrong Filter Setting is Used ...
All too often — filter settings are ignored. Different settings are typically used for monitoring when emphasis is placed on rhythm determination vs diagnostic mode, for which the focus is on interpreting 12-lead waveforms. Greater filtering is generally used in monitor mode, with a common setting beting between 0.5 Hz and 40 Hz. Doing so has the advantage of minimizing artifact and baseline wander that may affect rhythm interpretation. In contrast — a broader passband (typically from 0.05 Hz to 150 Hz) is recommended for diagnostic mode, where more accurate ST segment analysis is essential.
- I've taken Figure-2 from the illustration by García-Niebla et al (Rev Esp Cardiol 69(4):438, 2016) — to show how selection of a 40 Hz cutoff frequency (that is commonly chosen in clinical practice in an attempt to "improve" tracing appearance) may result in disappearance of fine ECG features such as the epsilon wave, that is only optimally seen in Figure-2 at a cutoff high-pass filter setting of 150 Hz (BLUE arrows).
-USE.png) |
| Figure 2: Illustration of the effect of filter settings on the likelihood of seeing epsilon waves on a standard 12-lead ECG. |
Reason #2: The Wrong Lead System is Used ...
I strongly recommend the section by Drs. Buttner and Cadogan in Life-In-The-Fast-Lane on the Fontaine Lead — https://litfl.com/fontaine-lead/ — as this concise review outlines what to know for optimizing your chance of identifying an epsilon wave in a patient with ARVD on ECG. I highlight below a few KEY points from this LITFL Review: - Identification of epsilon waves is potentially a most specific ECG sign of ARVD. These small deflections may be seen as a "blip" or "wiggle" either at the end, or just after the QRS complex. They are best seen in leads V1,V2 — and a bit less well seen in V3,V4.
- LITFL cites a figure of 23% for the frequency of visualizing epsilon waves on a standard ECG. The filter settings used in association with this figure are not mentioned — so given the tendency of all-too-often selecting a 40 Hz high-pass setting (instead of the optimal 150 Hz setting) — an even lower likelihood of finding epsilon waves might be expected on the ECGs sent our way in search of epsilon waves.
- In contrast — use of special placement of standard ECG machine electrodes called Fontaine Lead Placement — allowed detection of epsilon waves in up to 75% of patients! Rather than reproducing the user-friendly instructions on the LITFL site — I'll refer interested readers directly to their site — https://litfl.com/fontaine-lead/ —
- Finally —There are a variety of potential epsilon wave shapes! These include: i) "Wiggle" waves; ii) Small upward spikes; iii) Small downward spikes; and/or, iv) Smooth potential waves at the end of the QRS (which result in prolongation of the QRS in lead V1 exceeding duration of the QRS in lead V3 by ≥25 msec.).
How Large and Well-Defined Can Epsilon Waves Be?
Most of the examples of epsilon waves that I have seen show relatively small deflections. Because notation of filter settings is so commonly omitted from the ECGs sent my way — it's impossible to say how much of an effect suboptimal filter settings may have had on this smaller size of these epsilon wave deflections.
- In today's case — notation of filter settings was absent. That said — Dr. Nossen's magnified view with RED arrows on one of the subsequent ECGs clearly indicate a prominent epsilon wave deflection (seen best in lead V3).
On occasion — epsilon waves can be large and extremely well defined. The ECG in Figure-3 (taken from THIS CASE) — provides the BEST illustration of epsilon waves that I have seen. - The rhythm in Figure-3 is sinus — as evidenced by regular upright in lead II P waves, with a constant and normal PR interval. The QRS complex is wide, with QRS morphology consistent with RBBB/LAHB.
- Note that there is T wave inversion in the anterior leads, as should be expected with ARVD (albeit the presence of RBBB itself could account for some of this anterior T wave inversion).
- KEY Point: The reason for the bizarre shape of the QRS complex in lead V1 — is that the QRS in this lead is being prolonged by a huge Epsilon wave (dark BLUE arrow).
- To assist in looking for Epsilon waves in other leads — I dropped a vertical dark BLUE time-line through the peak of the huge Epsilon wave in lead V1 — extending downward through the long lead II rhythm strip at the bottom of the tracing. Doing so defines the point in the 2 simultaneously-recorded long lead rhythm strips that marks the occurrence of the Epsilon wave.
- Using this reference point we defined for the Epsilon wave in the long lead II and lead V1 rhythm strips — I then extended upward a vertical light BLUE time-line to highlight the expected location of any Epsilon waves that might be seen in simultaneously-recorded leads I,II,III — aVR,aVL,aVF — and V4,V5,V6.
- The light BLUE arrow in lead II highlights a surprisingly large negative Epsilon wave that is present in this lead.
- Following these upward extended light BLUE time-lines — we can see that smaller, but definitely-present negative Epsilon waves are also seen in leads I, aVL, aVF, and V3-thru-V6.
- Another positive Epsilon wave is seen in lead aVR.
-USE.png) |
| Figure 3: Epsilon waves in multiple leads! |

.png)














.png)





-USE.png)
-USE.png)
-USE.png)