An elderly woman had sudden SOB and 911 was called. Medics found her with labored breathing and 75% saturations. She was put on high flow oxygen. After placing her in the ambulance, she had a PEA arrest. She was intubated and ventilated, and given compression decompression CPR with the ResQPod and ResQPump.
Aside: these 2 devices were invented by researcher Keith Lurie, who is in the Department of EM here at Hennepin; this is the only method of CPR ever proven in a randomized trial to improve outcome in cardiac arrest see this ResQTrial, published in Lancet in 2011: Treatment of out-of-hospital cardiac arrest with an impedance threshold device and active compression decompression cardiopulmonary resuscitation improves survival with good neurological outcome: results from the ResQTrial.
This research team at Hennepin, which also includes Johanna Moore (Dept of EM) is now both studying and implementing compression decompression CPR with additional head up CPR, and a new head up CPR device called the Elegard. See this study of head up CPR in porcine model: Controlled sequential elevation of the head and thorax combined with active compression decompression cardiopulmonary resuscitation and an impedance threshold .
Read more about the Elegard here at EMS world: Raises Head, Looks Around: The State of Elevated CPR
Case continued
After 2 doses of epinephrine, ROSC was achieved.
The patient arrived intubated and with severe pulmonary edema.
Here was the first ECG:
Now there is second degree AV block (P-wave not conducted 3 times). The ST depression is less.
30 minutes later (time = 60 minutes):
After this, the patient was taken for angiogram:
Successful temporary transvenous pacemaker placement
Severe multivessel coronary artery disease that includes 90% stenosis of
the mid RCA, severe stenoses of the ostial and proximal circumflex, chronic total
occlusion of the distal LAD, and possible hemodynamically significant
stenosis of the distal left main
In the setting of transient heart block following PEA arrest, severe RCA
stenosis was treated as a possible contributor
Formal Echo:
Regional wall motion abnormality-inferior
Regional wall motion abnormality-inferolateral.
Peak troponin I was over 10,000 ng/L, consistent with OMI.
ECG after PCI:
And 3 days later:
The patient had complete neurologic recovery.
She was considered a poor candidate for Coronary Bypass and thus would be managed medically with or without additional less invasive coronary intervention.
===================================
MY Comment by KEN GRAUER, MD (10/27/2021):
===================================
Fascinating case (!) by Dr. Smith — fortunately with a positive ending. In the interest of responding to the questions raised by David Richley — I wanted to comment on the cardiac rhythm for the first 3 tracings.
============================
NOTE #1: As per Dr. Smith — this patient's AV block, whch developed following successful resuscitation — totally resolved with reestablishment of normal sinus rhythm following PCI. Therefore — I fully acknowledge that my "deep dive" on the cardiac rhythm is an academic exericse. That said — there are important lessons-to-be-learned regarding arrhythmia interpretation that will be clinically relevant for other cases.
============================
The 1st question that arose — was whether there was 1 or 2 P waves for each QRS complex in the 1st ECG of today's case (Figure-1).
- Although impossible to be certain of the rhythm from this single ECG in Figure-1 — the reason I immediately suspected that there might be 2:1 AV block, is that the PR interval is so long (ie, ~430 msec.), that it almost occurs in the middle of the R-R interval. Especially given the clinical setting (ie, shortly after ROSC) — AV blocks are common.
My Approach was as Follows:
- RED arrows in Figure-1 highlight definite sinus P waves.
- The WHITE arrow highlights slight notching (similar to the slight notching seen within the RED arrow P waves) — but this subtle notching is not seen at this same point in any of the other 9 QRS complexes.
- Although subtle — there is slight variation in the R-R interval, being just a little bit longer for the first R-R interval between beats #1-2 (which means that there is opportunity for the relative location of a P wave hiding within the QRS to "move" a little with respect to the QRS complex — as per the WHITE arrow).
- And — IF an extra P wave was hiding within the QRS complex — its location should be precisely midway between RED arrow P waves. The PINK arrows show how this is possible.
- NOTE #2: I did not yet know for certain that there was 2:1 AV block in this 1st tracing — because the findings I note above are subtle indeed. But I did strongly suspect it! — and subsequent tracings proved me to be correct.
- PEARL #1: All bets are off regarding the cardiac rhythm during a resuscitation (or post-resuscitation) setting. "With code rhythms — the heart simply does not read the textbook". As a result, in this clinical setting — you can see anything, and AV blocks are common.
 |
| Figure-1: The first ECG in today’s case. There is sinus tachycardia with 2:1 AV block (See text). |
Then came the 2nd ECG — and as per Dr. Smith, some form of 2nd-degree AV block was now obvious. But — What kind of 2nd-degree AV block was present?
- For clarity — I display the long lead II rhythm strip from ECG #2 with my proposed laddergram in Figure-2. But I immediately suspected this mechanism the moment I saw this tracing.
My Approach was as Follows:
- RED arrows in Figure-2 highlight sinus P waves. Although some P waves are once again hidden (at least in part) by QRS complexes — there are several places in which we clearly see 2 definite sinus P waves in a row! IF you set calipers at precisely this P-P interval — you can walk out perfectly regular sinus P waves throughout the tracing (RED arrows in Figure-2).
- PEARL #2: Note that the P-P interval for sinus P waves in Figure-2 is just over 2 large boxes in duration, which corresponds to a sinus tachycardia rate of ~130/minute. IF you return to Figure-1 — you'll note that the rate of the RED and PINK arrows I drew is exactly the same (ie, 130/minute) — and since ECG #2 was obtained just 30 minutes after ECG #1 — this essentially proves that the rhythm in ECG #1 was 2:1 AV block!
- Returning to My Approach to the rhythm in Figure-2. Although the ventricular rhythm is not regular — there is group beating! By this I mean that the shorter R-R intervals — and the longer R-R intervals (ie, between beats #1-2; 5-6 and 7-8) are also the same. PEARL #3: Whenever you see group beating — strongly consider the possibility of some form of Wenckebach block.
- Note that there are repetitive PR intervals in this tracing. That is — the PR intervals before beats #2, 6 and 8 are the same!
- Calipers tell us that the PR intervals before beats #3,4,5; 7 and 9 are also all the same — albeit slightly longer than the PR intervals preceding beats #2,6,8. The fact that there are 2 sets of repetitive PR intervals tells us that there is conduction (and that there is conduction with an increase in PR interval ...).
- Note that there is an extra non-conducted P wave between each of the longer R-R intervals in Figure-2. This is what suggested a dual-level of Wenckebach conduction to me, occurring at 2 levels within the AV node (DOTTED line within the AV Nodal Tier in the laddergram). Drawing the laddergram allowed me to prove this theory.
 |
| Figure-2: I've labeled P waves in ECG #2 — and added my proposed laddergram below the rhythm strip (See text). |
Then came the 3rd ECG. To me — this was the most complex tracing, because this post-resuscitation rhythm "simply does not obey the rules ... ". This 3rd ECG is not simple 2:1 AV block (Figure-3).
- As shown by the RED arrows — sinus P waves are once again regular at the same atrial rate of ~130/minute. But something is changing ...
- As I portray in the laddergram — I believe the first 4 beats represent a similar dual-level Wenckebach pattern as we saw for the longer R-R intervals in the laddergram for Figure-2. This explains why there are 3 P waves for each QRS complex for these first 4 beats in Figure-3. Note that the PR interval remains constant before the first 4 QRS complexes.
- However — Note that the PR interval changes before beats #6 and 7. This is easiest to see if you focus the the P waves labeled "b" and "c" — which clearly show a changing relationship to their neighboring QRS (ie, to beats #6 and 7).
- Note that the R-R interval gets longer at the end of ECG #3 (from 1240 msec. at the beginning of the tracing — to 1320, and then 1400 msec. at the end of the tracing). I do not know why ... Perhaps there is development of transient complete AV block with junctional escape beats? — or perhaps simply a change in the PR interval during Wenckebach conduction?
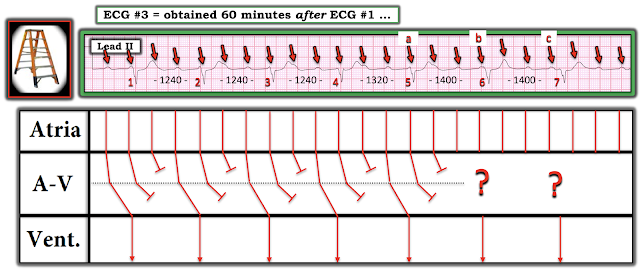 |
| Figure-3: I've labeled P waves in ECG #3 — and added my proposed laddergram below the rhythm strip (See text). |
In Conclusion: I thought this series of rhythms was fascinating. Even though I was unable to elucidate the specific mechanism for the 3rd tracing — the clinical points to emphasize are:
- AV blocks are common in the setting of cardiac arrest — and these types of AV block "do not always obey the rules".
- Always consider the possibility of 2:1 AV block whenever you see PR prolongation with P waves consistently seen near the middle of the R-R interval.
- Recognition of group beating and 2 or more repetitive PR intervals should suggest some form of Wenckebach conduction.
- Various forms of AV Wenckebach that arise in association with acute MI (and/or cardiac arrest) may resolve when the acute ischemic process is controlled. Despite what seemed to be severe 2nd-degree AV block — no pacemaker was ultimately needed for this patient.
- P.S. — IF interested in learning more on how to read and/or draw Laddergrams — CLICK HERE —






I think the ECG[30 minutes later (time = 60 minutes)] is 3:1 AV block with a P wave buried in R wave?
ReplyDeleteHello JJ. Please take ANOTHER LOOK at this blog post — See My Comment (at the bottom of the page) which I added just this morning (Oct. 27). I take a DETAILED LOOK at the rhythm for the first 3 tracings, and explain my assessment with laddergrams. Please let us know if you still have questions after reviewing My Comment. THANK YOU for your interest in Dr. Smith's ECG Blog! — :) Ken Grauer, MD
DeleteSorry, but I think in ECG named "30 minutes later (time = 60 minutes)" it is not AV block 2:1, but 3:1 or even complete AV block with some type of rescue rhythm (P rate is near 150 bpm)
ReplyDeleteAnd in ECG named
"30 minutes later, another ECG was recorded" it is not only P waves not conducted more than 3 times (may be it is 2:1-3:1 conduction?)
Or am I seeing something wrong?
Thank you for this great case, and all you work, and this exellent blog - I've been reading it for many years, it helps a lot in my work. Best regards, dr Anna Cherniakova from Russia :)
Hello Anna. Please take ANOTHER LOOK at this blog post — See My Comment (at the bottom of the page) which I added just this morning (Oct. 27). I take a DETAILED LOOK at the rhythm for the first 3 tracings, and explain my assessment with laddergrams. Please let us know if you still have questions after reviewing My Comment. THANK YOU for your interest in Dr. Smith's ECG Blog! — :) Ken Grauer, MD
Delete