Written by Pendell Meyers, edits by Steve Smith
A 52 year old female with history of hypothyroidism and smoking presented to the ED with an episode of chest pain that began suddenly around 1500 while sitting down at work. She states it felt like a central chest pressure that radiated to her jaw. The pain had been persistently present since since 1500 (seen at 1615 in the ED), but had waxed and waned in severity, with the initial onset of pain being the worst. She had dyspnea and diaphoresis when the pain began. Coworkers called EMS who administered aspirin and NTG, which the patient says did not relieve her pain. During initial exam, she reports that her dyspnea had improved, but she had new nausea and vomiting x2 while in triage.
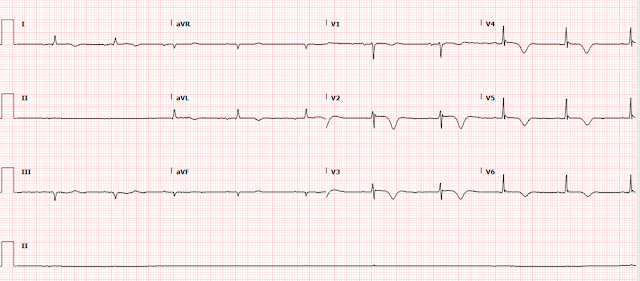
Here is her triage ECG at 1615:
 |
| What do you think? |
Smith comment (blinded to all information): This ECG, even without an old one for comparison, is diagnostic of LAD occlusion. T-waves like this are NEVER normal and only caused by transmural ischemia.
Her baseline ECG was available on file:
This baseline normal ECG proves that that first ECG above shows hyperacute T waves in leads V3-6, as well as likely hyperacute T waves in II, III, and aVF when compared to baseline. These T waves are evidence of acute transmural injury in the anterolateral and likely apical LV walls, which would fit well with acute LAD OMI. There is also abnormal STE in V2-V4 which is minimal in amplitude and does not meet STEMI criteria. Please notice that an experienced electrocardiographer can diagnose these T waves in V3-V5 as definitively hyperacute without having the baseline ECG to compare to, but with the baseline in hand everyone can see that these T waves are truly hyperacute throughout the precordium and the inferior leads.
According to the OMI progression of ECG findings, this is perhaps the earliest possible diagnosis of LAD OMI on ECG, with the maximal benefit to emergent reperfusion.
The ECG was not recognized as OMI. The first high sensitivity troponin I returned at 1647 elevated at 124 ng/L (reference limit less than 12 ng/L for women, less than 20 ng/L for men).
A second troponin was ordered, which resulted at 1903 at 530 ng/L.
It seems that a repeat ECG was ordered due to the rising troponins, at 1911:
At this time, 3 hours after arrival, we now see resolution of hyperacute T waves, with V2 and aVL showing inverted T waves likely indicative of spontaneous (lucky) reperfusion.
However, it seems that the patient had ongoing chest pain at this time, because she was given 4mg morphine and 4mg ondansetron for ongoing chest pain at 1945.
Another ECG was performed at 2007:
At this time, the providers start to notice the T wave inversions in aVL. They performed a bedside echo which showed an anterior and apical wall motion abnormality.
A third troponin resulted at 2025 at 987 ng/L.
With ongoing pain, rising troponin, and wall motion abnormality, the providers rightfully consulted cardiology for the possibility of emergent angiogram despite lack of STEMI criteria.
The cardiologist stated: "During my interview, patient is pain-free and resting comfortably after receiving morphine. Troponin has subsequently risen to 530 followed by 987. Patient remains pain-free fortunately."
This sentence seems to suggest that the cardiologist believes that morphine is a reasonable response to ongoing ischemic symptoms instead of reperfusion. This reflects the practice I have seen at many institutions, and cases I am sent from all over the world.
Despite documenting that the pain is all gone, the cardiologist immediately orders nitroglycerin paste at 2046.
The fourth troponin results at 2142 at 1108 ng/L.
Enoxaparin ordered at 2149.
More nitroglycerin ordered at 2341. Who orders repeat doses of NTG at midnight on a regular medicine floor for patients who are asymptomatic? Despite national guidelines that require emergent angiogram for ongoing ACS, we have orders for ischemic symptoms without any documentation of whether or not the patient has ongoing pain.
The fifth troponin returns at 0105 at 1150 ng/L, and no more will be ordered.
Smith comment: A rising troponin does NOT necessarily mean that the artery remains occluded. Infarction that was ongoing hours ago can result in rising troponin now. Only the combination of BOTH 1) resolution of ECG findings (present here) AND 2) with resolution of symptoms (apparently absent here, as patient required morphine and nitroglycerin) can tell you that the ischemia is resolved.
The next morning at 0800, an ECG is recorded:
 |
| Findings consistent with LAD reperfusion. |
And another at 0900:
 |
| Deepening of T-wave inversion. This is the typical progression after reperfusion. |
Catheterization was performed the next day 0935
"There is severe apical hypokinesis with EF estimated at 40%. The circumflex and RCA are within normal limits. There was a focal lesion in the midportion of the LAD after 2nd perforator which had the appearance of a likely coronary dissection. There was a significant apical LAD vessel beyond this area. There was a wall motion abnormality consistent with infarction in this distribution.
It was elected to attempt intervention (stenting) on this area primarily due to the size of the vessel and the short area of the dissection.
The LAD lesion was estimated at 80%. There was no pre-intervention TIMI flow listed. Post-intervention TIMI flow was 3.
During cardiac rehab clinic follow up 10 days later, the patient states in a questionnaire that she can walk around her house, do light work including washing dishes, but states that she is unable to walk a block on level ground, unable to climb a flight of stairs, unable to rake leaves, or participate in sports.
Here is her ECG at that visit:
Her long term outcome is unknown, but we know that NSTEMI patients with missed OMI have double the short term,1-year, and 2-year mortality according to data by Khan et al who metaanalyzed over 40,000 NSTEMI patients in RCTs. And that's just their MORTALITY, not to mention their long term decreased quality of life, CHF, etc.
Luckily for this patient, however, she appears to have reperfused after a few hours of occlusion, and the ECG does not show progression to full thickness infarct (there is preservation of R waves, and reperfusion T waves). Hopefully her EF and cardiac function will improve.
Here is the OMI progression with a yellow arrow showing the course that this patient's ECGs followed in this case:
Learning Points:
Hyperacute T waves can be learned and recognized. They are symmetric, fat, broad based, encroaching on the QRS, resulting in large area under the curve of the ST segment and T wave compared to baseline.
Learn the OMI progression.
Missed or delayed care for OMI carries a much worse prognosis. Luckily for this patient she spontaneously reperfused in the early stages of missed OMI.
I hear many people say that coronary dissections do not receive PCI. This is a false and dangerous assumption. You cannot know until angiogram whether it will be suitable for PCI, and type I ACS (plaque rupture and thrombosis) is vastly more common as a cause of OMI.






By the way, the first ECG displays a tiny bit of STE in V4-V5 compared to the baseline. But this can be easily missed...
ReplyDelete