A 30-something woman presented with a few days of feeling ill. She had a history of paroxysmal atrial fibrillation, bio-prosthetic mitral valve, and tricuspid valvuloplasty, and was on Coumadin.
Records showed she is usually in sinus rhythm and has normal LV function.
She presented hypotensive (systolic pressure 80), with diffuse B lines, flat IVC, good LV function, and an irregular, fast heart beat.
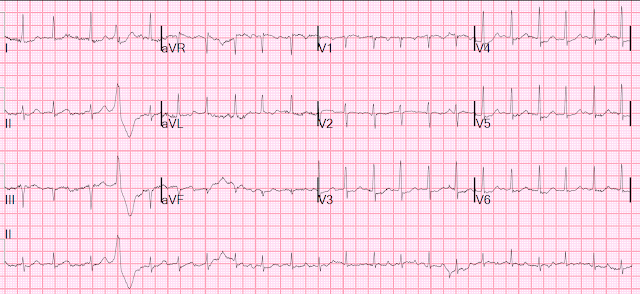
Here is here ECG:
Here is her POCUS:
What do you think?
There is a small LV with good function and a large left atrium, and moderately large RV.
There is another finding on the ultrasound which I'll explain below. Do you see it?
Her inferior vena cava was very flat, with respiratory variation, and she had diffuse bilateral B lines
Here is her chest X-ray:
This shows pretty severe pulmonary edema.
Questions:
1. Why does she have severe pulmonary edema, excellent LV function, a small LV, and a flat IVC?
2. What precipitated this acute emergency and why?
3. What do you want to do first?
Clinical Course
The paradoxes of this case were not immediately identified. At first they had thought, due to the flat IVC and good LV function, that she was septic with pneumonia (thus relatively volume depleted, interpreting the B-lines and X-ray as pneumonia rather than as pulmonary edema). Thus, they had given fluids and antibiotics. This management did not improve the pulmonary edema.
Comment:
Whether this is sepsis or not, if a patient is usually in sinus rhythm, but presents unstable (hypotension/shock and/or pulmonary edema and/or ischemic chest pain) in atrial fibrillation with RVR, then cardioversion is indicated, especially if the patient is anticoagulated (her INR was 8.8). Hypotension and pulmonary edema, no matter the etoliogy, will virtually always be improved with electrical cardioversion. Furthermore, in this case, because the patient is usually in sinus, the cardioversion is likely to be successful.
Improvement in clinical status is to be expected in sinus rhythm, vs. atrial fib, due to both the restoration of the atrial contribution to ventricular filling, and also potentially due to the slowing of the ventricular rate.
Clinical Course continued
I arrived late to the case, saw this situation, and said "we need to cardiovert."
The patient was given 10 mg of etomidate and cardiovereted at 200J; she converted to sinus rhythm and immediately felt better.
Comment: She did not seem to me to be septic, and so the hemodynamics were unusual, and the only way to explain the entire clinical picture was to postulate the there was worsening mitral stenosis, exacerbated by sudden atrial fibrillation:
1. Mitral stenosis leads to poor LV filling, which causes BOTH pulmonary edema AND hypotension but in the presence of good LV function and a small (poorly filled) LV. (All present in this case)
2. Atrial fib worsens the situation in 2 ways:
1) There is no atrial contribution to LV filling and
2) The rate is very fast, leaving little time for filling. When there is mitral stenosis, the flow from the left atrium to the LV is very slow and the LV needs more time to fill. Thus, a slower heart rate is beneficial.
3. Even in the presence of hypovolemia (flat IVC), a patient with severe mitral stenosis can have cardiogenic pulmonary edema.
Look again at the bedside echo. Here is a still photo:
____________
Contrast Echo
Left atrial enlargement.
Right atrial enlargement.
Right ventricular enlargement. Decreased right ventricular systolic performance .
Normal estimated left ventricular ejection fraction, 77%.
Bioprosthetic mitral valve with severe stenosis (see below).
Also: Mitral valve insufficiency-moderate, eccentric.
Pulmonary hypertension; estimated PA systolic pressure 65 mm Hg + RA.
Inferior vena cava is normal in size with respiratory variation.
ADDITIONAL REMARKS
Patient in sinus rhythm. Compared to the prior study, there is now evidence for severe, mixed stenosis/regurgitation involving the mitral bioprosthesis (placed in 2006), with markedly elevated mean transmitral gradient of 14 mmHg @ HR 102 bpm and accompanying pulmonary hypertension.
Comment: had this been done during atrial fib with RVR, the transmitral gradient would have been far greater!
The mitral prosthesis appears bulky with exaggerated motion throughout the cardiac cycle.
Mitral Valve
Area (PHT): 3.14 cm^2 Area (continuity): 1.3 cm^2
Peak E-Wave: 2.5 m/s Mean Velocity: 1.78 m/s
Peak A-Wave: 1.1 m/s Mean Gradient: 14 mmHg
Peak Gradient: 25 mmHg Deceleration Time: 238 msec
P1/2t: 70 msec
E/A Ratio: 2.36
Summary: Severe prosthetic valve mitral stenosis mean gradient 14 mmHg at heart rate 102 bpm and moderate MR.
____________________
The subsequent cardiology note explains everything very well:
"Past medical history significant for paroxysmal atrial fibrillation, rheumatic mitral stenosis status post bio-prosthetic MVR in 2006 now with evidence of prosthetic valve dysfunction with severe mitral stenosis and moderate mitral regurgitation and resultant RV enlargement and decreased systolic function with severe pulmonary hypertension. She presented to the ED with 2 weeks of weakness and decreased oral intake and 2 days of palpitations shortness of breath and orthopnea. She was found to be in atrial fibrillation with RVR. She was also volume depleted and hypotensive and received fluids. She underwent cardioversion in the emergency department after she developed pulmonary edema following volume resuscitation. It appears that she most likely had 1-2 weeks of a nondescript viral syndrome resulting in fatigue and decreased oral intake. She probably then developed atrial fibrillation with RVR in the last 1 to 2 days which, in the setting of severe mitral stenosis of her bioprosthetic mitral valve, resulted in symptoms of heart failure and flash pulmonary edema due to elevated left-sided filling pressures at a high heart rate. She markedly improved after cardioversion."
She was given beta blockade with metoprolol to slow the heart rate.
She will need a mitral valve replacement.




How can the MS be severe with a valve area more than 3 sq.cm both by PHT and continuity? Af with ventricular rate >100/min and significant Mr may result in a high gradient.
ReplyDeleteI just looked at a subsequent TEE and MR was more prominent than MS on that one. Good question.
DeleteThe more I read this blog, the more ignorant I feel.
ReplyDeleteIs it just me? 🤔
So sorry! There is just so much to learn. If you keep on working on it, you'll get there.
DeleteI always like your blog but I especially like these larger complete case reviews. Any recommendation for good sites similar to yours but for Ultrasound?
ReplyDeleteThanks for sharing!
I don't know of any quite like this. There is this one from my ED, but they don't keep posting very often. https://www.hennepinultrasound.com/
Delete