Which of the following 6 ECGs of patients with chest pain represent inferior OMI?
The answer could be 1 or more than 1.
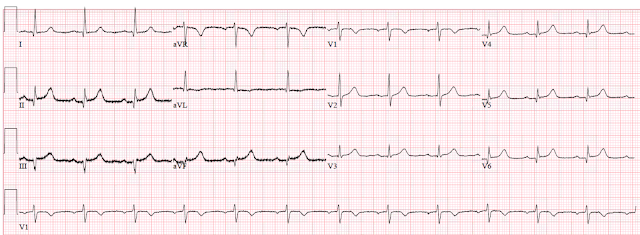
1.
2.
3.
4.
5.
6.
Answer:
3. and 5. are inferior OMI
1., 2., 4., and 6. are limb lead early repolarization
Is it really possible to differentiate these?
Yes. Pendell did it easily getting 6/6 correct.
I put this post up because I just received number 3 from a former graduate. It is from an otherwise healthy middle-aged male with 2 episodes of brief stuttering epigastric and chest pain on the day before, then presented with 2 hours of constant pain.
Let's look at it again:
Here is another from the same patient, slightly later, with arrows pointing out the hyperacute T-waves:
There is minimal inferior STE, but T-waves are massive in proportion to the QRS, there is ST depression, minimal, in aVL, and also some minimal ST depression in V4-V6.
The former resident activated the cath lab based on this ECG and, although the interventionalist was skeptical, he had experience with this ex-resident making some very good calls in the past and so he agreed.
There was a 95% thrombotic RCA lesion that was stented.
Finally, this is an extra one that I put on Twitter and Facebook to promote the post:
The answer could be 1 or more than 1.
1.
2.
4.
 |
| https://hqmeded-ecg.blogspot.com/2011/10/inferior-st-elevation-what-is-diagnosis.html |
5.
 |
| https://hqmeded-ecg.blogspot.com/2018/05/is-there-delayed-activation-wave.html |
6.
 |
| https://hqmeded-ecg.blogspot.com/2013/04/a-40-year-old-male-with-several-chronic.html |
Answer:
3. and 5. are inferior OMI
1., 2., 4., and 6. are limb lead early repolarization
Is it really possible to differentiate these?
Yes. Pendell did it easily getting 6/6 correct.
I put this post up because I just received number 3 from a former graduate. It is from an otherwise healthy middle-aged male with 2 episodes of brief stuttering epigastric and chest pain on the day before, then presented with 2 hours of constant pain.
Let's look at it again:
Here is another from the same patient, slightly later, with arrows pointing out the hyperacute T-waves:
There is minimal inferior STE, but T-waves are massive in proportion to the QRS, there is ST depression, minimal, in aVL, and also some minimal ST depression in V4-V6.
The former resident activated the cath lab based on this ECG and, although the interventionalist was skeptical, he had experience with this ex-resident making some very good calls in the past and so he agreed.
There was a 95% thrombotic RCA lesion that was stented.
Finally, this is an extra one that I put on Twitter and Facebook to promote the post:
 |
| The answer, with Ken's comments too, are at the post:An ECG sent to me with concern for hyperacute T-waves |
===================================
MY Comment by KEN GRAUER, MD (2/1/2020):
===================================
This is a challenging case. In it, we are shown 7 tracings (the first 6 are numbered — the 7th was added at the end by Dr. Smith as a final example). Each of these patients presented to the ED with chest pain. Of these 7 tracings — 3 represent acute inferior OMI; the other 4 do not.
- QUESTION #1: Which ECG findings are common among the 4 tracings that did not represent acute inferior OMI?
- QUESTION #2: Which ECG findings are common among the 3 tracings that did represent acute inferior MI?
ANSWER: I fully acknowledge that I was not certain that the 4 non-OMI tracings were the result of a repolarization variant. In particular — ECG #6 showed fairly dramatic ST elevation in multiple leads.
- We are not told details of the history in any of these cases — beyond knowing that these patients presented to the ED with chest pain.
- Sometimes, it simply is not possible to be 100% certain from a single ECG if it represents acute OMI or not.
- IF the clinical scenario in which the “chest pain” is experienced is “right” — then other diagnoses (ie, acute myopericarditis) may be possible — and acute myocarditis can present with an ECG picture virtually identical to acute OMI.
The above said — each of the 4 tracings that did not represent acute inferior OMI ( = ECGs #1, 2, 4, 6) have the following ECG findings in common:
- They lack the “magical” mirror-image reciprocal ST-T wave relationship that is usually seen between lead III and lead aVL in acute inferior OMI (See My Comment in the 8/9/2018 post and the 10/6/2018 post in Dr. Smith’s ECG Blog, among many other times we have emphasized this finding!).
- Leads V2 and V3 do not at all suggest acute posterior involvement.
- The shape of ST elevation is upward sloping.
- There is J-point notching or J-point slurring in at least a couple of leads.
- The QTc is relatively short.
- Large Q waves are absent.
- Even when ST-T wave elevation is fairly marked — it is not localized to the inferior leads in these 4 tracings that do not represent acute inferior OMI.
- KEY: None of the ECG findings in the above 7 bullets are absolute. Nevertheless — the points described in these 7 bullets highlight ECG findings we look for when trying to distinguish between repolarization variants vs acute inferior OMI.
WHAT ABOUT the 3 Tracings that DO represent Acute Inferior OMI? For clarity — I reproduce these 3 tracings in Figure-1.
- What ECG findings do these 3 examples of acute inferior OMI have in common?
- HINT: The same 6 KEY leads in each of these 3 tracings show similar abnormal findings!
 |
| Figure-1: The 3 tracings in this post that DO represent acute inferior OMI (See text). |
Each of the 3 tracings that do represent acute inferior OMI ( = ECGs #3, 5, 7) have the following ECG findings in common:
- The ST-T wave is abnormal in each of the 3 inferior leads. It should be noted that inferior MIs are sometimes quite subtle — a feature accentuated in ECG #3 and ECG #7, in which QRS amplitude in the inferior leads is quite modest. When the QRS complex is tiny (as it is in leads III and aVF in ECGs #3 and 7) — then the “amount” of ST elevation will not be great. This is why — SHAPE is more important than amount!
- Looking closer — the ST-T wave is clearly hyperacute in leads II, III and aVF in ECG #3 — and in leads III and aVF in ECG #7. By this, I mean that considering QRS amplitude — the T waves in these leads are taller-than-they-should-be and fatter-at-their-peak with a base that is wider-than-expected.
- Admittedly — the ST-T waves in ECG #5 do not look nearly as worrisome as they do in ECGs #3 and #7. That said — there is ST elevation in each of the 3 inferior leads in ECG #5 — and there are other clearly worrisome findings on this tracing.
- The “magical” mirror-image opposite ST segment picture is seen between leads III and aVL in all 3 of these tracings with acute inferior OMI ( = ECGs #3, 5 and 7). This is true even in ECG #5 — in which the shallow-but-real depressed ST segment in lead aVL is the mirror-image opposite of the subtle-but-real ST elevation in lead III.
- Finally — Leads V2 and V3 in each of the 3 tracings in Figure-1 with acute inferior OMI show clear abnormalities that strongly suggest associated acute posterior involvement. Although subtle — there is slight-but-real J-point ST depression (or at least ST segment flattening) in each of these leads, whereas normally there should be slight gently-upsloping ST elevation. In addition, the T waves in leads V2 and V3 in both ECG #3 and ECG #5 look hyperacute. Lastly — the QRS complex in lead V3 in each of these 3 tracings shows a taller-than-expected R wave, which is another finding consistent with posterior infarction (CLICK HERE — for illustration of this concept).
BOTTOM LINE: When looking to determine IF there is acute inferior OMI — the 6 KEY leads that I focus on are the 3 inferior leads ( = leads II, III and aVF) — lead aVL (looking for reciprocal ST-T wave depression that is the mirror-image opposite of what we see in lead III) — and anterior leads V2 and V3 (looking for suggestion of acute posterior involvement(.
- Each of the 3 tracings in Figure-1 show abnormal findings in each of these 6 KEY leads.
- Abnormal (more subtle) findings are also found in some additional leads — but it is the 6 KEY leads that provide the most important information when looking to determine IF there is acute inferior OMI.
- The more leads that are clearly abnormal — the greater the likelihood that a patient with chest pain is having an ongoing acute cardiac event. With the exception of leads aVR and V1 — virtually all of the other 10 leads in each of the 3 tracings in Figure-1 show at least ST-T wave flattening, straightening, or slight depression — and, some of these other leads also manifest hyperacute T waves.
Our THANKS to Dr. Smith for posting this illustrative case!






Great learning exercise! I have two things to mention...
ReplyDelete1. A rule that I teach all my students - which I call Jones's Rule - states that any ST depression on the ECG of a patient with chest pain credible for ACS is a RECIPROCAL CHANGE until proved otherwise. This is typically seen in aVL and II, III and aVF, but we normally concentrate on Leads III and aVL. Lead aVL is especially problematic because the QRS is often very small and the importance of its repolarization morphology is too often overlooked.
2) Subtlety and severity have no linear relationship. Just because a finding is very subtle (such as the ST depression in aVL in a few of these ECGs) does not mean that its importance and significance is small. Missing these subtle findings has resulted in too many unnecessary deaths from misdiagnosis.
Again, thanks for a great exercise!
THANKS so much Jerry. The 3 of us agree completely with your comment! The “saying” I would always use (as per the 1st bullet under my Figure-1) = “SHAPE is more important than amount” regarding ST-T wave changes — :)
Delete