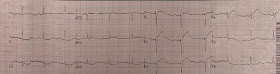
An ECG was texted to me (Smith) without any clinical information:
My answer:
"This is classic for PE, but it can also be present in any hypoxia due pulmonary hypoxic vasoconstriction and resulting acute pulmonary hypertension and acute right heart strain. This is NOT Wellens. Is the patient hypoxic? SOB?"
The answer was yes. This clinical information followed: "The patient had a COPD exacerbation with a prehospital SpO2 of 60%. He had respiratory failure, was intubated, and was diagnosed with pneumonia."
Some providers were worried about ACS because of this ECG.
My answer alleviated their concern for ACS and no further workup was done for ACS.
4 important features that indicate acute right hear strain:
1. Tachycardia (or nearly)
2. S1Q3T3
3. Poor R-wave progression
4. Domed T-wave inversion
5. Most important: T-wave inversion not only in precordial leads, but also in lead III.
See more in-depth discussion at the bottom.
It turns out there was a previous ECG for comparison, which I did not see for weeks afterwards:
Other similar cases of acute right heart strain
See this case of asthma whose ECG mimics acute PE:
And some similar ECGs from Pulmonary Embolism:
And an Acute PE mimic due to chronic pulmonary hypertension and right ventricular hypertrophy:
 |
| What did I say? |
My answer:
"This is classic for PE, but it can also be present in any hypoxia due pulmonary hypoxic vasoconstriction and resulting acute pulmonary hypertension and acute right heart strain. This is NOT Wellens. Is the patient hypoxic? SOB?"
The answer was yes. This clinical information followed: "The patient had a COPD exacerbation with a prehospital SpO2 of 60%. He had respiratory failure, was intubated, and was diagnosed with pneumonia."
Some providers were worried about ACS because of this ECG.
My answer alleviated their concern for ACS and no further workup was done for ACS.
4 important features that indicate acute right hear strain:
1. Tachycardia (or nearly)
2. S1Q3T3
3. Poor R-wave progression
4. Domed T-wave inversion
5. Most important: T-wave inversion not only in precordial leads, but also in lead III.
See more in-depth discussion at the bottom.
It turns out there was a previous ECG for comparison, which I did not see for weeks afterwards:
Other similar cases of acute right heart strain
See this case of asthma whose ECG mimics acute PE:
Is it pulmonary embolism?
And some similar ECGs from Pulmonary Embolism:
And an Acute PE mimic due to chronic pulmonary hypertension and right ventricular hypertrophy:
The ECG in Pulmonary Embolism:
This ECG was classic for acute hypoxia, which includes acute PE, so here is some information on the ECG in acute PE:
The ECG is not sensitive for PE, but when there are findings such as S1Q3T3 or anterior T-wave inversions, or new RBBB, or sinus tachycardia, then they have a (+) likelihood ratio. S1Q3T3, or even just the T3, may help to differentiate Wellens' from PE.
What is an S1Q3T3? Very few studies define S1Q3T3. It was described way back in 1935 and both S1 and Q3 were defined as 1.5 mm (0.15 mV). In the Marchik article, (assuming they defined it the same way, and the methods do not specify this), among patients with suspicion for PE, S1Q3T3 was found in 8.5% of patients with PE and 3.3% of patients without PE.
When there is a positive troponin, then the findings are related to myocardial injury, and then PE and MI are at the top of the differential, and Kosuge's article (see below) applies.
Kosuge et al. showed that, when T-waves are inverted in precordial leads, if they are also inverted in lead III and V1, then pulmonary embolism is far more likely than ACS. In this study, (quote) "negative T waves in leads III and V1 were observed in only 1% of patients with ACS compared with 88% of patients with APE (p less than 0.001). The sensitivity, specificity, positive predictive value, and negative predictive value of this finding for the diagnosis of PE were 88%, 99%, 97%, and 95%, respectively. In conclusion, the presence of negative T waves in both leads III and V1 allows PE to be differentiated simply but accurately from ACS in patients with negative T waves in the precordial leads."
Witting et al. looked at consecutive patients with PE, ACS, or neither. They found that only 11% of PE had 1 mm T-wave inversions in both lead III and lead V1, vs. 4.6% of controls.
This does not contradict the conclusions of Kosuge et al., who studied a select population of patients who were known to have either PE or ACS -- that is, all were indeed ill. Of those select patients, the ones who also had T-wave inversions in the right precordial leads were studied. Of these, T-wave inversion in lead III was very specific for PE. In my experience, this is true, but needs validation in a study of similar methodology. Supporting Kosuge, Ferrari found that anterior T-wave inversions were the most common ECG finding in massive PE.
Finally, Stein et al. found normal ECGs in only 3 of 50 patients with massive PE, and 9 of 40 with PE that is not massive. Today, however, that number would be lower because we diagnose more of the smaller PEs that have minimal symptoms.
Finally, Stein et al. found normal ECGs in only 3 of 50 patients with massive PE, and 9 of 40 with PE that is not massive. Today, however, that number would be lower because we diagnose more of the smaller PEs that have minimal symptoms.
This is a paper worth reading: Marchik et al. studied ECG findings of PE in 6049 patients, 354 of whom had PE.
Just to be clear: these are all patients being evaluated for PE, whereas Kosuge studied those with only ACS and PE left on the differential. We should apply Kosuge's data to our case here because of the positive troponin.
They found the following positive likelihood ratios for PE:
1. S1Q3T3 = 3.7
2. Inverted T-waves in V1 and V2, = 1.8
3. Inverted T-waves in V1-V3, = 2.6
4. Inverted T-waves in V1-V4, = 3.7
4. Inverted T-waves in V1-V4, = 3.7
5. Incomplete RBBB = 1.7
6. Tachycardia, = 1.8.
Finally, they found these independent predictors of PE:
In our case here, there is S1Q3T3, precordial T-wave inversions with inversion in lead III, and tachycardia (rate 96 can be classified as tachycardia). All together, that makes for a very high odds ratio, but as we can see from this case, it is not specific for PE, rather for acute hypoxia.
Ken Grauer's comments follow.
Although I usually agree with Ken, I do not necessarily agree with all of what he writes, but his perspective is always interesting and helpful.
He thinks this ECG is not classic for acute right heart strain. I do, and his arguments below have not changed my mind.
What does it mean when I write that the ECG is "classic" for PE?
It means that if you see this pattern, you better think of and investigate PE or other causes of acute hypoxia because they are very high on the differential. "Classic" is not the same thing as pathognomonic; this ECG is not pathognomonic (although close).
As you can see, without any clinical information, I diagnosed acute hypoxia from the ECG alone, without any doubts.
===================================
MY Comment by KEN GRAUER, MD (2/6/2020):
===================================
Excellent case presented by Dr. Smith for highlighting many KEY aspects regarding ECG recognition of acute Pulmonary Embolism (Acute PE).
- I agree completely with Dr. Smith that: i) the ECG in this case ( = ECG #1 in Figure-1) is not suggestive of acute MI; ii) that some History is needed for optimal clinical ECG interpretation; and, iii) that the moment I learned that this patient presented with ECG #1 in association with acute dyspnea and profound hypoxemia — that I felt a diagnosis of acute PE needed to be strongly considered.
That said — I do not think ( = my opinion) that ECG #1 is necessarily “classic” for acute hypoxemia (of which acute PE can be one of the causes).
- To explain my opinion — I’ve added ECG #2 to Figure-1, which is taken from the March 12, 2018 post on Dr. Smith’s ECG blog — in which this woman in her 40s with progressively worsening dyspnea was found to have massive acute PE.
 |
| Figure-1: The ECG in this case that was texted to Dr. Smith — compared to the presenting ECG from the March 12, 2018 post, in which massive acute PE was confirmed (See text). |
My THOUGHTS: Many excellent points are highlighted by Dr. Smith in this case. These points have been emphasized in many previous posts on Dr. Smith’s blog (See the April 5, 2019 post, including My Comment at the bottom of that page).
- KEY: In an adult with new-onset dyspnea or pleuritic (or atypical) chest pain — the finding of anterior T wave inversion will much more often be due to acute PE than to acute coronary disease. This is especially true IF there is also inferior T wave inversion (in leads II, III and aVF) — which is the other lead area that characteristically manifests ST-T wave changes of acute RV “strain”.
PEARL: Rather than any single ECG finding — RVH patterns (including acute RV “strain”) are what I call the “Detective Diagnosis” — in that there is no single ECG finding that is absolutely diagnostic — but instead, there is a series of clues, that like a good “detective story”, when put together lead to strong suggestion of the clinical diagnosis.
- The patient in this case presented with profound hypoxemia + an S1Q3T3 pattern (at least in some complexes) + anterior T wave inversion (extending in ECG #1 to lead V5) + T wave inversion in lead III — so as per Dr. Smith, a series of ECG clues consistent with acute PE are present in ECG #1, in this patient who presents with profound hypoxemia.
That said — Reasons I did not feel ( = my opinion) that the diagnosis of acute PE was definite after seeing ECG #1 included the following:
- While the clinical history of acute dyspnea with profound hypoxemia is certainly consistent with acute PE — many patients with longstanding end-stage COPD but without acute PE may present with exacerbations associated with profound hypoxemia, that sometimes necessitates intubation. So, the history in this case is consistent but not necessarily indicative of acute PE.
- The heart rate in ECG #1 is more rapid than usual (ie, ~85-90/minute) — but not “tachycardic”. Many patients with acute COPD exacerbations present with a similar heart rate.
- There is much baseline artifact. This makes interpretation of ST-T wave morphology challenging in the other two inferior leads (ie, leads II and aVF). Given beat-to-beat baseline variation and ST-T wave morphology variation — I did not feel we could say there was clear ST depression or T wave inversion in either lead II or lead III. Therefore — T wave inversion in ECG #1 is limited to lead III.
- QUESTIONS (that I do not know the answer to): What does the literature say about the predictive value of T inversion isolated to lead III? — compared to those cases in which all 3 inferior leads showed ST-T depression/inversion? Was this looked at in the studies that were done?
- Lead III in ECG #1 manifests beat-to-beat variation in QRS morphology. It is true that at least 2 of the 4 complexes in lead III manifest Q waves (I thought there was probably an initial r wave in the 1st complex in lead III) — and it is true that the T wave is inverted in each of the 3 complexes we see in lead III. But it is also true that: i) T wave inversion in lead III is a natural consequence of incomplete RBBB patterns that are sometimes seen in this right-sided lead; ii) T wave inversion is expected normally, when there is a predominantly negative QRS complex (ie, the QS complex we see in Figure-1) in lead III; and, iii) The S wave in lead I is deeper when there is an incomplete RBBB equivalent in lead III (Isn’t the s wave so very shallow for the 2nd complex in lead I — which corresponds to the QS in lead III?). One might interpret those deeper S waves in lead I as the terminal s wave expected to be seen with incomplete RBBB. BOTTOM Line: While I fully acknowledge that the above points are extremely “picky” (and that many readers may not agree with me) — My view is that there is not a “clean” S1Q3T3 pattern in ECG #1, and in my opinion the diagnostic value of this finding is therefore reduced in this case.
- More than just “poor R wave progression” — there is almost no R wave at all in leads V1, V2 and V3 (if not some “loss” of R wave between V1-to-V2). The ECG of most patients with longstanding pulmonary disease show more r wave progression than I see in ECG #1. This made me consider the possibility of prior anterior infarction with residual ST segment coving + T wave inversion.
- No prior ECG is shown in this case. I would have loved to know IF this patient had a prior anterior MI.
- Other findings of acute RV “strain” are really not seen in ECG #1. There is no RAA (Right Atrial Abnormality) — no right axis — no atrial abnormalities.
- Finally — the same Kosuge group whose ECG findings on the diagnosis of acute PE are summarized above emphasized that in patients with precordial lead T wave inversion — the predictive value of chest lead T wave inversion for acute PE is greatest when the maximal amount of T wave inversion is seen in leads V1,V2 (Kosuge et al, JACC 67: 528, 2016). Their conclusion: “Among patients with acute PE vs ACS who had T inversion in V1-4, peak negative T wave in leads V1-2 simply but accurately differentiates acute PE from ACS”. The greatest amount of T wave inversion is not seen in leads V1,V2 in ECG #1. Instead — T inversion is at least as deep in leads V3-5 as it is in V1,V2.
BOTTOM Lines: Let me emphasize that I completely agree that precordial lead ST segment coving with fairly deep, symmetric T wave inversion in this patient with profound hypoxemia merits strong consideration of acute PE until this possibility is either ruled in or ruled out! That said — I do not think ECG #1 is diagnostic by itself of acute PE (nor do I think we can necessarily attribute everything we see in ECG #1 to hypoxemia on the basis of this single ECG).
- What can be stated — is that ECG #1 is definitely not suggestive of an acute MI. That said — the possibility of a prior anterior MI with some residual ST-T wave changes can not be excluded without more information from looking at ECG #1 alone.
- What can also be stated — is that ECG #1 is not Wellens' Syndrome because: i) the history is wrong (ie, there is no mention of prior chest pain); ii) Wellens T waves imply that loss of anterior forces from infarction has not yet occurred (ie, Wellens implies that anterior R waves are still preserved) — and this is not the case in ECG #1; and, iii) Symmetric T wave inversion (as seen in ECG #1) is not specific for distinguishing Wellens from other causes of T wave inversion (ie, there is no overly steep downslope to the T waves in ECG #1).
Now Take a Look at ECG #2: As mentioned earlier, ECG #2 is taken from a woman in her 40s with a more specific history suggesting acute PE (this tracing is taken from the March 12, 2018 post in Dr. Smith’s blog). I thought the history in this case + ECG #2 were more diagnostic of acute PE because:
- There is definite sinus tachycardia in ECG #2.
- There is an acute RV “Strain” pattern with ST depression/T wave inversion in both inferior and anterior leads (Note dramatic ST-T wave changes in II, III and aVF — as well as V3,V4).
- There is RAA (tall, peaked and pointed P waves in each of the inferior leads).
- There is an SI, SII, SIII pattern (one usually does not see S waves in all 3 standard leads).
- There is persistence of S waves through to lead V6.
- Compared to ECG #1 — Note that there is progressive increase in R wave amplitude in ECG #2 as one moves across the chest leads. This was lacking in ECG #1 (which is why I considered previous anterior MI in ECG #1).
- PEARL: I suspect there is a lead placement problem with lead V2 in ECG #2. It just doesn’t make physiologic sense to have deep T wave inversion in V1 and V3, but not in V2. This is important to the overall picture in ECG #2, because acute RV strain should produce anterior T wave inversion (and lacking this in V2 just doesn’t “fit”, unless that lead was malpositioned).
- Finally — Note that the S1Q3T3 pattern is missing in ECG #2, despite documentation of a massive PE. This is not surprising, since overall sensitivity of this ECG finding is low (ie, many patients with documented acute PE will not have an S1Q3T3 pattern).
Our THANKS to Dr. Smith for presenting this instructive case! (P.S.: Wish I knew more about what happened to the patient with ECG #1 ... ).