Post by Smith and Meyers
Sam Ghali (https://twitter.com/EM_RESUS) just asked me (Smith):
"Steve, do left main coronary artery *occlusions* (actual ones with transmural ischemia) have ST Depression or ST Elevation in aVR?"
Smith and Meyers answer:
First, LM occlusion is uncommon in the ED because most of these die before they can get a 12-lead recorded.
But if they do present:
The very common presentation of diffuse STD with reciprocal STE in aVR is NOT left main occlusion, though it might be due to subtotal LM ACS, but is much more often due to non-ACS conditions, especially demand ischemia. In these cases, STE in aVR is always reciprocal to the ST depression of subendocardial ischemia elsewhere (ST depression vector towards II and V5).
Total LM occlusion can present with STE or STD in aVR.
When total LM occlusion does present with STE in aVR, there is ALWAYS ST Elevation elsewhere which makes STEMI obvious; in other words, STE is never limited to only aVR but instead it is part of a massive and usually obvious STEMI.
The pattern seen may, or may not, be unique to left main occlusion. Some total LAD occlusion manifest on the ECG similarly to some left main occlusions. All are, however, clearly massive STEMI.
To reiterate the most important part relevant to your question: LM occlusion does not present with isolated STE in aVR. Depending on where the STE vector of the LM occlusion shows up on the ECG, there may be either STE, or STD, or neither in aVR, and lead aVR will not be the important part of the ECG interpretation in these cases.
Below are 6 anecdotal cases of true complete left main occlusion with no collateral circulation:
3 have STE in aVR
1 has no ST shift in aVR
2 have STD in aVR
The ECG can have a variety of presentations in LM Occlusion. Here I explain:
At the bottom of the post, I have re-printed the section on aVR in my article on the ECG in ACS from the Canadian Journal of Cardiology:
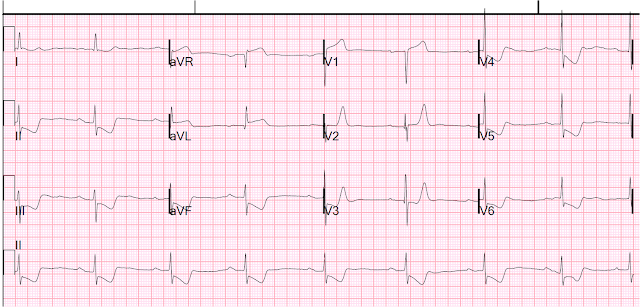
Chris Mondie of the Newark Beth Israel Emergency Medicine Residency sent case 1 below of a 100% LM occlusion. His comments/questions are inserted below the ECG:
A 50-something woman presented with 3 days of intermittent chest pain that became worse on the day of presentation, with diaphoresis and radiation to the left arm, as well as abdominal pain.
This is her ECG:
The cath lab was activated and a 100% left main occlusion was found.
Chris' comments/questions:
"Every "ST elevation in aVR" case I've ever seen has been triple vessel, insufficiency, or demand/global subendocardial ischemia secondary to some underlying sepsis/increased metabolic demand."
"My question is this: we are taught that aVR elevation with diffuse ST depression can be indicative of LMCA."
Smith: this teaching is incorrect; see this post: ST Elevation in Lead aVR, with diffuse ST depression, does not represent left main occlusion.
"In my case above there is indeed significant STE in aVR as well as V1, there is also STE in aVL and V2 which seems to violate the "diffuse STD" claim.... Why is it that we
don't see lateral STE in the classically taught "STE in aVR, and diffuse STD". If the lesion is so proximal, wouldn't we normally expect to see lateral STE instead of STD in the lateral leads?"
Smith response to case: "It is not surprising that this ECG was from a patient with acute LM occlusion." and I sent him the above ST vector explanation.
Case 3.
Sam Ghali (https://twitter.com/EM_RESUS) just asked me (Smith):
"Steve, do left main coronary artery *occlusions* (actual ones with transmural ischemia) have ST Depression or ST Elevation in aVR?"
Smith and Meyers answer:
First, LM occlusion is uncommon in the ED because most of these die before they can get a 12-lead recorded.
But if they do present:
The very common presentation of diffuse STD with reciprocal STE in aVR is NOT left main occlusion, though it might be due to subtotal LM ACS, but is much more often due to non-ACS conditions, especially demand ischemia. In these cases, STE in aVR is always reciprocal to the ST depression of subendocardial ischemia elsewhere (ST depression vector towards II and V5).
Total LM occlusion can present with STE or STD in aVR.
When total LM occlusion does present with STE in aVR, there is ALWAYS ST Elevation elsewhere which makes STEMI obvious; in other words, STE is never limited to only aVR but instead it is part of a massive and usually obvious STEMI.
The pattern seen may, or may not, be unique to left main occlusion. Some total LAD occlusion manifest on the ECG similarly to some left main occlusions. All are, however, clearly massive STEMI.
To reiterate the most important part relevant to your question: LM occlusion does not present with isolated STE in aVR. Depending on where the STE vector of the LM occlusion shows up on the ECG, there may be either STE, or STD, or neither in aVR, and lead aVR will not be the important part of the ECG interpretation in these cases.
Below are 6 anecdotal cases of true complete left main occlusion with no collateral circulation:
3 have STE in aVR
1 has no ST shift in aVR
2 have STD in aVR
The ECG can have a variety of presentations in LM Occlusion. Here I explain:
First, you don't know for certain what the state of the artery was at the time of the ECG.
It might have been (barely) open but closed at the time of angiography.
That said, complete LM occlusion would be expected to have subepicardial ischemia (STE) in these myocardial territories:
STE vector
1. The anterior direction (anterior) due to LAD (STE in V2-V4, possibly V5, V6)
2. The lateral direction (leftward) due to:
2a. D1 (STE I, aVL, V5, V6) and
2b. Circumflex (STE in I, aVL V4-V6)
3. The septum (rightward) from LAD (STE in aVR, V1, reciprocal ST depression in V4-V6)
The ST elevation from (2.) above may cancel out or reverse both the reciprocal STD in V4-V6 and the STE in V1 and aVR.
The ST elevation from (2.) above may cancel out or reverse both the reciprocal STD in V4-V6 and the STE in V1 and aVR.
4. Posterior (due to circumflex occlusion) (ST depression in anterior leads)
This ST depression may cancel out the STE in anterior leads!
This ST depression may cancel out the STE in anterior leads!
5. Superior due to subepicardial ischemia of the small part of the base of the heart which is directed superior (STE in V1, aVL, aVR)
This may result in ST depression in inferior leads
This may result in ST depression in inferior leads
Each ST vectors will have different contributions in different patients. They will add up in varying magnitudes resulting in a variety of ECG presentations.
At the bottom of the post, I have re-printed the section on aVR in my article on the ECG in ACS from the Canadian Journal of Cardiology:
New Insights Into the Use of the 12-Lead Electrocardiogram for Diagnosing Acute Myocardial Infarction in the Emergency Department
Case 1.
A 50-something woman presented with 3 days of intermittent chest pain that became worse on the day of presentation, with diaphoresis and radiation to the left arm, as well as abdominal pain.
This is her ECG:
 |
| An obvious STEMI, but which artery? ST elevation in aVR |
The cath lab was activated and a 100% left main occlusion was found.
Chris' comments/questions:
"Every "ST elevation in aVR" case I've ever seen has been triple vessel, insufficiency, or demand/global subendocardial ischemia secondary to some underlying sepsis/increased metabolic demand."
"My question is this: we are taught that aVR elevation with diffuse ST depression can be indicative of LMCA."
Smith: this teaching is incorrect; see this post: ST Elevation in Lead aVR, with diffuse ST depression, does not represent left main occlusion.
"In my case above there is indeed significant STE in aVR as well as V1, there is also STE in aVL and V2 which seems to violate the "diffuse STD" claim.... Why is it that we
don't see lateral STE in the classically taught "STE in aVR, and diffuse STD". If the lesion is so proximal, wouldn't we normally expect to see lateral STE instead of STD in the lateral leads?"
Smith response to case: "It is not surprising that this ECG was from a patient with acute LM occlusion." and I sent him the above ST vector explanation.
Case 2.
Here is another proven left main occlusion in a young woman who presented with sudden pulmonary edema, had this ECG recorded, then arrested and was resuscitated after 30 minutes of CPR:
This pattern of RBBB/LAFB was also the most common pattern in Fiol et al. (ref 64 below) case series of 7 total LM occlusions.
See this paper by Widimsky et al, which shows the high association of RBBB, especially with LAFB, with LAD occlusion. Furthermore, among 35 patients with acute left main coronary artery occlusion, 9 presented with RBBB (mostly with LAFB) on the admission ECG.
Widimsky P et al. Primary angioplasty in acute myocardial infarction with right bundle branch block: should new onset right bundle branch block be added to future guidelines as an indication for reperfusion therapy?
Case 3.
Here is another total left main:
Total eclipse of the heart -- written by Pendell
 |
| ST Depression in aVR |
And with lines to point out the end of the QRS:
 |
| ST Depression in aVR |
Case 4.
Here is another 100% left main that was contributed by Rohin Francis of Medlife Crisis (https://twitter.com/MedCrisis)
 |
| ST depression in aVR |
Here is the angiogram from Rohin's case:
Case 5.
Here is a 95% Left Main with TIMI-1 flow:
Here is the angiogram:
 |
| Black arrows are very narrowed left main, red arrow is LAD with flow, and yellow arrow is circumflex with flow. |
Case 6.
Beware crescendo angina in patient with known CAD
 |
| ST Elevation in aVR |
Case 7.
Another left main occlusion, but this one shows subendocardial ischemia. Why?
 |
| LM is indeed 100% occluded |
But the RCA angiogram shows that there are RCA collaterals supplying subepicardial flow to other territories:
 |
| All the flow on the upper right is flowing from the RCA into the LAD territory |
Case 8.
______________
The below section is copied from my article in the Canadian Journal of Cardiology:
New Insights Into the Use of the 12-Lead Electrocardiogram for Diagnosing Acute Myocardial Infarction in the Emergency Department
Lead AVR in Acute Coronary Syndromes (61)
Many experts consider the ECG pattern of STE in aVR, with diffuse ST
depression elsewhere (referred to here as the “aVR STE pattern”), to be representative
of left main (LM) OMI.(7) The 2013 ACC/AHA STEMI guidelines consider this a “STEMI equivalent,” where thrombolytic therapy is not contraindicated (Evidence level B, no
specific class of recommendation).(16) However, these conclusions are based on studies
where LM lesions were not true subtotal or complete occlusion (i.e. TIMI 0/1 flow).(61,62) The interventional community defines occlusive LM disease as >50% by FFR, or ≥75%
stenosis,(63) but urgent or emergent intervention on lesions not meeting these thresholds
is only imperative if it is a thrombotic lesion and the patient has refractory ischemic
symptoms (i.e. not resolved by nitrates, antiplatelet, and antithrombotic therapies). (See
3 examples in appendix: Figure S7a, S7b and S7c) Although nearly half of patients with ≥1 mm STE in aVR due to ACS will require
coronary artery bypass surgery for revascularization,(61) the infarct artery is often not the
LM, but rather the LAD or severe 3-vessel disease. More importantly, such ECG
findings are frequently due to non-occlusive etiologies (E.g. baseline LVH, demand
ischemia secondary to respiratory failure, aortic stenosis, hemorrhagic shock). Knotts et
al. found that only 23% of patients with the aVR STE pattern had any LM disease (fewer
if defined as ≥ 50% stenosis). Only 28% of patients had ACS of any vessel, and, of
those patients, the LM was the culprit in just 49% (14% of all cases).(56) It was a baseline
finding in 62% of patients, usually due to LVH.
Thus, a number of expert reviews emphasize the low specificity of the aVR STE
pattern, preferring to label it as circumferential subendocardial ischemia; in this
syndrome, STE in aVR is reciprocal STE, reciprocal to an ST depression vector towards
leads II and V5.(8,10,61) The aVR STE pattern is also not sensitive for LM OMI. On the other hand,
anterior STEMI with combined new right bundle branch block and left anterior fascicular
block is highly suggestive of LM OMI.(64 65) (See example 12-lead in appendix: Figure
S8)
It should be re-emphasized that true LM OMI (i.e. TIMI flow 0) is rare in the ED,
as most either die before arrival or are recognized clinically due to cardiogenic shock.
Thus, reported specificities of STE in aVR for LM OMI result in very low positive
predictive values. Of those who do get to the ED, many present with clear STE.(65, 64, 61) The ACC/AHA states that thrombolytics are not contraindicated for diffuse STD
“associated with” STE in aVR. Given the poor specificity of this pattern for LM OMI, we
suggest that thrombolytics should only be considered for those with profound ST
depression that is clearly due to ACS, is refractory to all other medical management,
and only when PCI is completely unavailable.
Lead aVR in STEMI
Some patients whose ECGs already meet conventional STEMI criteria may also
have STE in lead aVR. This finding does not alter the need to pursue emergent
reperfusion, although it may suggest a poorer prognosis.(61,66) In a patient with otherwise
diagnostic STE, additional STE in aVR does not represent LM OMI and is not helpful in
diagnosing the infarct-related artery or the site of occlusion.(67) Less than 3% of anterior
STEMI has LM OMI, and most are recognized clinically due to cardiogenic shock. (68, 69)
Finally, there is one series of left main total occlusion in the literature (reference 64), and it, too, had 7 cases. Below is one paragraph from that publication, which also starts the introduction stating that most LM total occlusions do not survive, and that only 3 of these 7 survived:
"To our knowledge, no series describing LMT occlusion (TIMI flow = 0) with a STEMI pattern has been published in the literature. We found that the most typical ECG pattern in our small series was the one described in proximal occlusion of a long LAD, consisting of ST elevation in the precordial leads from V2 to V4 through V6 and in leads I and aVL, as well as ST depression in the inferior leads16 and often with RBBB and LAH (LAFB). In complete occlusion of the LMT, there is involvement of the left circumflex coronary artery, which generates ST depression in V1 and aVR, and consequently attenuates ST elevation in both leads. This causes the lack of ST changes in V1 and aVR that are frequently found in total occlusion of a long LAD. However, we have to remember that in cases of proximal LAD occlusion before the first septal branch, ST elevation is not always present in V1 (despite LAD occlusion proximal to the first septal perforator) if there exists a large conal branch of the right coronary artery (RCA)17t hat perfuses the high septum together with the first septal branch. This double perfusion of the high septum provides protection from ischemia. Patients with LMT occlusion who survive usually present with a very dominant RCA and a poor hemodynamic state when compared with those with LAD proximal occlusion."
References
7. Rokos IC, French WJ, Mattu A, et al. Appropriate cardiac cath lab activation:
optimizing electrocardiogram interpretation and clinical decision-making for acute STelevation myocardial infarction. American heart journal 2010;160:995-1003, .e1-8.
16. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the
management of ST-elevation myocardial infarction: a report of the American College of
Cardiology Foundation/American Heart Association Task Force on Practice Guidelines.
Journal of the American College of Cardiology 2013;61:e78-140.
61. Smith SW. Updates on the Electrocardiogram in Acute Coronary Syndromes.
Current Emergency and Hospital Medicine Reports 2013;1:43-52.
62. Jong GP, Ma T, Chou P, Shyu MY, Tseng WK, Chang TC. Reciprocal changes in
12-lead electrocardiography can predict left main coronary artery lesion in patients with
acute myocardial infarction. International heart journal 2006;47:13-20.
63. Stone GW, Sabik JF, Serruys PW, et al. Everolimus-Eluting Stents or Bypass
Surgery for Left Main Coronary Artery Disease. The New England journal of medicine
2016;375:2223-35.
64. Fiol M, Carrillo A, Rodriguez A, Pascual M, Bethencourt A, Bayes de Luna A.
Electrocardiographic changes of ST-elevation myocardial infarction in patients with complete occlusion of the left main trunk without collateral circulation: differential
diagnosis and clinical considerations. J Electrocardiol 2012;45:487-90.
65. Widimsky P, Rohac F, Stasek J, et al. Primary angioplasty in acute myocardial
infarction with right bundle branch block: should new onset right bundle branch block be
added to future guidelines as an indication for reperfusion therapy? European heart
journal 2012;33:86-95.
66. Kukla P, Bryniarski L, Dudek D, Krolikowski T, Kawecka Jaszcz K. Prognostic
significance of ST segment changes in lead aVR in patients with acute inferior
myocardial infarction with ST segment elevation. Kardiologia polska 2012;70:111-8.
67. Kosuge M, Ebina T, Hibi K, et al. An early and simple predictor of severe left
main and/or three-vessel disease in patients with non-ST-segment elevation acute
coronary syndrome. The American journal of cardiology 2011;107:495-500.
68. Zoghbi GJ, Misra VK, Brott BC, et al. ST Elevation Myocardial Infarction Due To
LEFT Main Culprit Lesions: Percutaneous Coronary Intervention Outcomes. Journal of
the American College of Cardiology 2010;55:A183.E1712.
69. Kurisu S, Inoue I, Kawagoe T, et al. Electrocardiographic features in patients with
acute myocardial infarction associated with left main coronary artery occlusion. Heart
(British Cardiac Society) 2004;90:1059-60.





Clarifies an extremely frequent misunderstanding about aVR STE. Will give this link to read to all the people that insist aVR is LM occlusion. Thanks Steve!
ReplyDelete