A middle-aged man presented with 7-8/10 non-radiating chest tightness to the left chest wall, associated with nausea but no diaphoresis, that began while walking approximately 40 minutes prior to arrival at the ED. The pain resolved as he arrived to the emergency department. He had 2 episodes over the past 2 days of similar chest tightness. He had a history of hypertension but stopped taking his medication several years ago. The patient is pretty sure that this discomfort was his reflux.
BP was 200/100.
Here was his triage ECG. It is uncertain if the patient was pain free at this time or not, or, if pain free, for how long he had been pain free. He was definitely pain free by the time of arrival at his ED room.
With a newly upright T-wave, one must consider pseudonormalization and re-occlusion. In fact, that would be most likely. Even if the patient is pain free, as this patient was (he felt fine).
See this case: Why we need continuous 12-lead ST segment monitoring in Wellens' syndrome
But this ECG does not look like an LAD occlusion. Moreover, an echo showed no wall motion abnormality.
This was my interpretation: although most ischemic T-wave inversion is post-ischemic like Wellens, sometime active ischemia results in isolated T-wave inversion. In such cases, if there is no infarction (necrosis), when the ischemia resolves, the T-wave may normalize (in contrast to Pseudo-normalize). When this happens, troponins are negative, there is no wall motion abnormality, and it is true unstable angina. (Wall motion abnormalities may also occasionally quickly resolve in Wellens syndrome if the infarct is very small and the ischemia brief).
Case continued
All troponins were negative. The patient underwent a stress echo, which was MARKEDLY positive. The angiogram showed a 95% LAD stenosis and a 70% stenosis of the first diagonal off the LAD (LADD1).
Here is the post-PCI ECG, 2 days later:
Comment
Imagine this scenario:
The patient did not get his ECG at triage. Rather, it was not recorded until he arrived at his room. The ECG could have been completely normal. He has negative troponins. He thinks it is his reflux. His HEART score would have been 3 (low) and he would be discharged. His EDACS score would have been 14 (low risk).
Learning Points:
1. Unstable Angina still exists
2. Chest pain scores can result in discharge of a high risk patient.
3. The ECG is essential, and recording it at triage can avoid missing a diagnostic moment.
4. T-wave inversion can be due to acute non-infarct ischemia, in which case it can reverse and normalize. Troponins are negative and it is thus "unstable angina."
5. T-wave inversion can be post-ischemic. If it is, the troponins are positive and the T-wave inversion evolves to become deeper and deeper.
Other posts
 |
| What do you think? |
This appears to be a classic Wellens' ECG, Pattern A, with terminal T-wave inversion in V2-V4, preserved R-waves, and it appears to be Wellens' syndrome, as it occurred after resolution of typical angina pain.
We assumed this was Wellens' syndrome and treated as such.
Wellens' syndrome represents the aftermath of an unrecorded occlusion (STEMI) with spontaneous reperfusion. Wellens' waves are "reperfusion T-waves" and are identical to the T-waves seen after therapeutic reperfusion. If true Wellens', they always are associated with slightly elevated troponin and always evolve over the next 12-72 hours into Pattern B waves (deep, symmetric). If they do not evolve in this manner, it is not true Wellens'.
Wellens syndrome requires that the pain be resolved and the R-waves are preserved. (In other words, the artery was occluded but has sponteneously reperfused, resulting in pain relief)
Wellens syndrome requires that the pain be resolved and the R-waves are preserved. (In other words, the artery was occluded but has sponteneously reperfused, resulting in pain relief)
It is important to monitor patients with Wellens' syndrome for re-occlusion, which is usually, but not always, associated with recurrent chest pain. Re-occlusion results in the T-wave becoming upright again (T-wave pseudonormalization).
We treated him with aspirin and heparin and metoprolol.
The patient remained pain free. Repeat BP was 140/80. 90 minutes later, another ECG was recorded:
With a newly upright T-wave, one must consider pseudonormalization and re-occlusion. In fact, that would be most likely. Even if the patient is pain free, as this patient was (he felt fine).
See this case: Why we need continuous 12-lead ST segment monitoring in Wellens' syndrome
But this ECG does not look like an LAD occlusion. Moreover, an echo showed no wall motion abnormality.
This was my interpretation: although most ischemic T-wave inversion is post-ischemic like Wellens, sometime active ischemia results in isolated T-wave inversion. In such cases, if there is no infarction (necrosis), when the ischemia resolves, the T-wave may normalize (in contrast to Pseudo-normalize). When this happens, troponins are negative, there is no wall motion abnormality, and it is true unstable angina. (Wall motion abnormalities may also occasionally quickly resolve in Wellens syndrome if the infarct is very small and the ischemia brief).
Case continued
All troponins were negative. The patient underwent a stress echo, which was MARKEDLY positive. The angiogram showed a 95% LAD stenosis and a 70% stenosis of the first diagonal off the LAD (LADD1).
Here is the post-PCI ECG, 2 days later:
Comment
Imagine this scenario:
The patient did not get his ECG at triage. Rather, it was not recorded until he arrived at his room. The ECG could have been completely normal. He has negative troponins. He thinks it is his reflux. His HEART score would have been 3 (low) and he would be discharged. His EDACS score would have been 14 (low risk).
Learning Points:
1. Unstable Angina still exists
2. Chest pain scores can result in discharge of a high risk patient.
3. The ECG is essential, and recording it at triage can avoid missing a diagnostic moment.
4. T-wave inversion can be due to acute non-infarct ischemia, in which case it can reverse and normalize. Troponins are negative and it is thus "unstable angina."
5. T-wave inversion can be post-ischemic. If it is, the troponins are positive and the T-wave inversion evolves to become deeper and deeper.
Classic Evolution of Wellens' T-waves over 26 hours
Other posts
Dynamic T-wave inversion (apparent Wellens' waves), all troponins negative: Unstable Angina
Subtle Dynamic T-waves, Followed by LAD Occlusion and Arrest
Subtle LAD Occlusion with Pseudonormalization of Wellens' Waves.
Pseudonormalization of T-waves
==================================
Comment by KEN GRAUER, MD (12/14/2018):
==================================
Interesting case that brings up a number of important concepts regarding Wellens’ Syndrome. For clarity — I’ve reproduced the first 2 ECGs in this case in Figure-1.
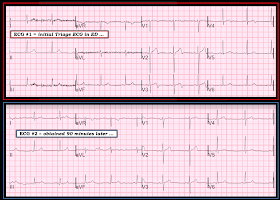 |
| Figure-1: The first 2 ECGs in this case (See text). |
==========================
It is certainly possible that IF the timing had been such that this patient’s initial ECG was normal (as it was for ECG #2 in Figure-1) — that the severity of this patient’s underlying coronary disease could have been overlooked. I’d add the following points:
- I’ve always thought of Wellens' Syndrome as a way to predict high likelihood of a tight, proximal LAD lesion. True, Wellens' Syndrome is seen before a large anterior infarction has occurred — thus, there should be preservation of anterior R waves. Therefore, the classic Wellens’ ECG Pattern A seen in ECG #1, with steep terminal downsloping T waves and terminal T wave negativity in one or more anterior leads, given the history in this case of intermittent (now resolved) worrisome chest pain — IS highly predictive of proximal LAD narrowing. That’s why the team diagnosed Wellens’ Syndrome, and began treating accordingly.
- In contrast, the isolated ECG finding of deep, symmetric chest lead T wave inversion doesn’t fit my definition ( = My Opinion) of what true Wellens’ Syndrome is — because there are other potential causes of deep, symmetric T wave inversion (ie, cardiomyopathy; ischemia not related to proximal, high-grade LAD narrowing; prior infarction; etc.). Of course, if this Pattern B of deep, symmetric T wave inversion occurs in a patient with the expected history AND follows an initial ECG showing the typical Pattern A — then, this would be consistent with the typical evolution of true Wellens’ Syndrome.
- In this particular case, the history of new-onset, worrisome chest pain (that then resolved) + classic Wellens' Pattern A terminal T wave inversion with preserved anterior R waves in the initial (triage) ECG is definitive for a need to assume severe LAD disease until proven otherwise — almost regardless of what the next ECG might show.
- Normalization of terminal T wave activity in the ECG #2 in this case constitutes a dynamic ST-T wave change. Even if troponins are negative and infarction is not documented — dynamic ECG changes in association with new chest discomfort is indication for investigation.
- Chest Pain scores can be misleading. Such scores all include subjective assessment of the patient's history, as well as at least some subjectivity in ECG assessment. As has been emphasized on numerous blog posts on this site — more than a single tracing will usually be needed for optimal diagnosis whenever the slightest of doubt regarding acuity exists. The onus of proof that chest discomfort in a patient who presents to the ED is not cardiac rests on the clinician (What brought this patient to the ED at this particular moment?). Especially when a single initial ECG is not obviously abnormal, and an initial troponin is negative — the accuracy of a chest pain score depends more than ever on the accuracy of assessing the subjective component of the patient’s symptoms.



Dr. Smith and co-
ReplyDeleteExcellent post as always. What caught my eye this time was that you listed the patient's HEART score. Is this something you regularly use in your ED workup? (Backstory: the EMS agency I work for recently participated in the PARA-HEART study through Wake Forest Baptist, in which we implemented a prehospital HEART score as well as a troponin into our chest pain care.) And if you do use it regularly, what are your thoughts on its efficacy?
Thanks,
Doug (EMT-P)
Doug,
DeleteI do not use it regularly, but sometimes. But I use it here because many reflexively use it without thinking about when it may result in a false negative.
Steve Smith