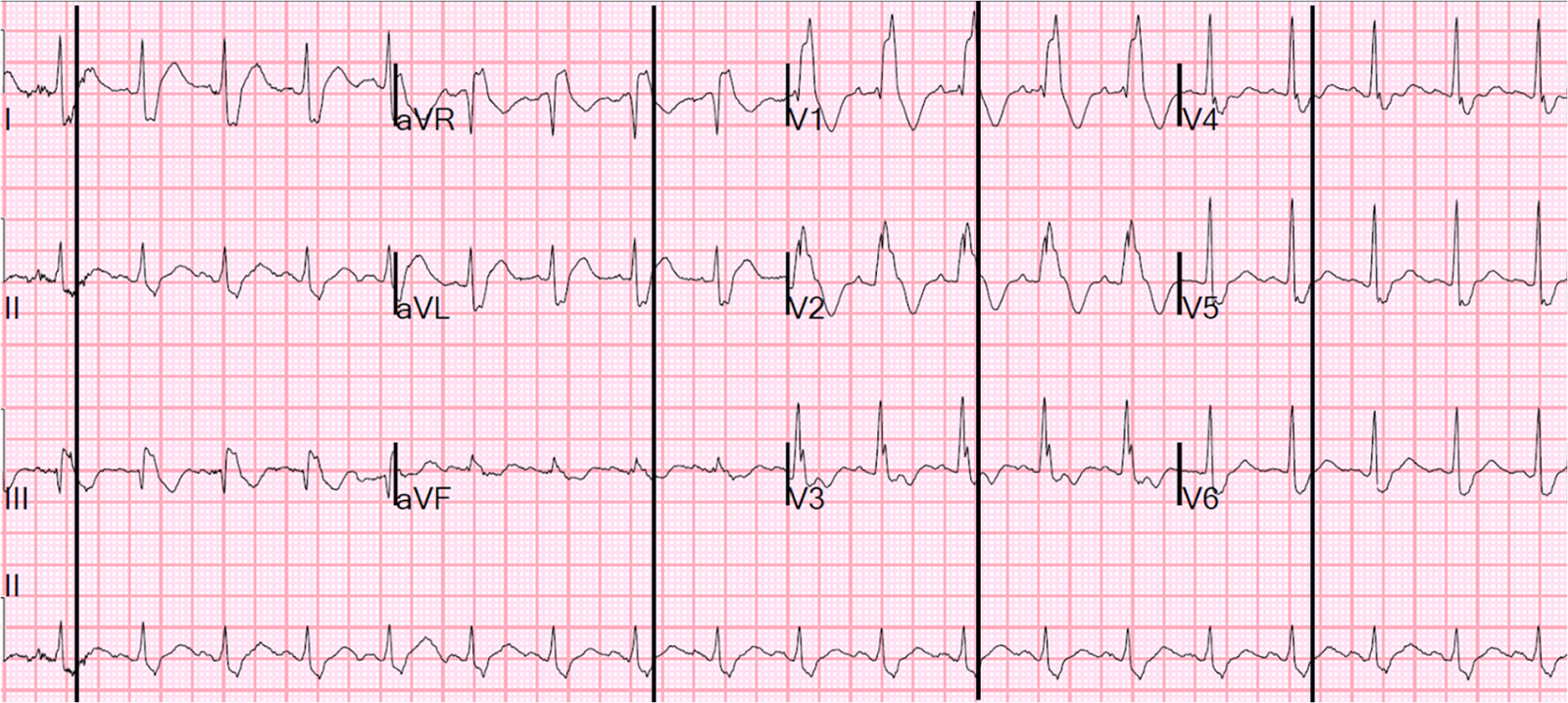
Case 2. A middle-aged male with h/o CAD and stents presented with typical chest pressure. Here is his ECG:
 |
| The resident was alarmed at the "ST elevation in III with reciprocal ST depression in aVL" Are you alarmed? |
This is a very common misread.
It may be difficult to read STEMI in the setting of RBBB. The trick is to find the end of the QRS.
The so-called "ST Elevation" is really the end of the QRS of Right Bundle Branch block. The QRS duration is slightly long even for RBBB, at 166 ms. I draw the end of the QRS here:
Case 2. An elderly patient with a ruptured abdominal aortic aneurysm:
 |
| Formal ECG Interpretation (final read in the chart!): "Inferior ST elevation, lead III, with reciprocal ST depression in aVL." What do you think? |
Answer:
What appears to be ST elevation and depression is simply a squared off part of the end of the QRS, which is long due to RBBB.
Case 3:
Male in 30's with chest pain, cough, and fever. He has clinical pneumonia. Called 911.
This ECG was recorded prehospital, and the computer read STEMI, so the medics activated the cath lab:
 |
| What do you think? |
Here is the same ECG with lines drawn through the J-point (end of QRS, beginning of ST segment), which is best seen in leads V4-V6:
But the clinical history is not compatible with STEMI, so one must be very cautious about the ECG interpretation.
The medics activated the cath lab.
The patient arrived in the ED and had this ECG recorded:
 |
| Interpretation? |
Analysis by finding the end of the QRS, beginning of ST segment (J-point):
 |
| Again, there is ST elevation in I and aVL (though barely any in V2), and reciprocal ST depression in III. The ECG is consistent with high lateral STEMI. |
A bedside ultrasound was done by the emergency physician, using Speckle Tracking. Unfortunately, that video is unavailable.
It appeared to show a lateral wall motion abnormality. RBBB does not affect wall motion by dyssynchrony in the way that LBBB does.
Here is a parasternal long axis without speckle tracking:
There is very good function, but the lateral wall is not in this view.
30 minutes later, this ECG was recorded:
 |
| There is less high lateral ST elevation |
And another 3.5 hours later, this one:
 |
| All ST elevation is gone |
The patient was treated for pneumonia and ruled out for MI.
--Does he need a stress test?
--Is there likely to be fixed coronary stenosis that led to demand ischemia during pneumonia?
--Was the ST elevation due to transient demand ischemia, or is it false positive?
Unfortunately, I don't know the answer to those questions, but this ST elevation should be assumed to be ischemic until proven otherwise.
Case 4.
A male in late middle age with a history of RCA stent 8 years prior complained of chest pain. EMS recorded the following ECG:
 | |
|
There is RBBB and LAFB (it is new compared to the previous), which can make it difficult to see the end of the QRS. I have annotated it here:
 | |
|
See this paper by Widimsky et al, which shows the high association of RBBB, especially with LAFB, with LAD occlusion. Furthermore, among 35 patients with acute left main coronary artery occlusion, 9 presented with RBBB (mostly with LAFB) on the admission ECG.
Here are three more dramatic cases that illustrate RBBB + LAFB
Case 1 of cardiac arrest with unrecognized STEMI, died.
Case 2 with 68 minutes of CPR and good outcome
Case 3 with LAD occlusion, cardiac arrest, could not be resuscitated
Case Progression
In order to keep patient confidentiality, I will only give the barest of follow up:
As the emergency physician was immediately assessing the patient, he had a v fib arrest. He could not be resuscitated in the ED but was taken to the cath lab while on LUCAS (mechanical) CPR, underwent successful PCI of a proximal LAD occlusion during chest compression, and after opening the artery, achieved ROSC (return of spontaneous circulation).



excellent as usual dr smith
ReplyDeleteThank you, Ioannis!
ReplyDeleteThanks to you dr.
ReplyDeleteRegarding pneumonia in 30 years old, EKG ischaemic findings points to an underlying CAD , may be 40 to 50 percent lesion in LAD. Pneumonia caused anoxia, causing ST elevation. May be a smoker, diabetic.
ReplyDeleteI suggested that:
Delete"The patient was treated for pneumonia and ruled out for MI."
"--Does he need a stress test?
--Is there likely to be fixed coronary stenosis that led to demand ischemia during pneumonia?
--Was the ST elevation due to transient demand ischemia, or is it false positive?"
However, even if this is demand ischemia, not ACS, one would expect troponins to rise, which they did not.