A 30-something presented with chest pain, palpitations, and SOB. He has had similar symptoms for 4 years, but has never been evaluated.
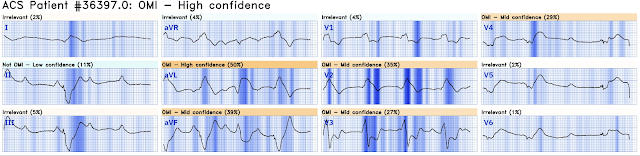
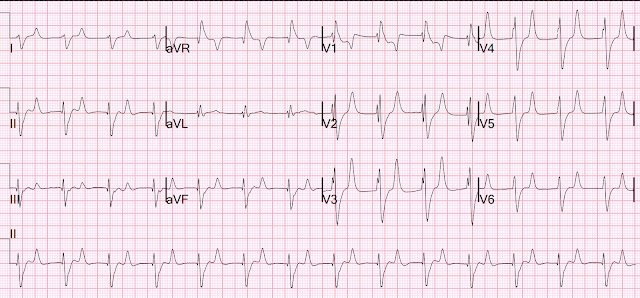
Here is his presenting ECG, which was sent to me real time, along with the 2nd ECG below:
Shortly after arrival, the patient spontaneously converted to this rhythm (also sent to me, along with the first):
The two ECGs above were texted to me with the text: "Young Guy came in in SVT but now in and out of irregular wide complex tachycardia. -- not sure if polymorphic VT vs. a fib with WPW."
My response: "Definitely not polymorphic VT. Definitely atrial fibrillation. Probably WPW but is very slow for atrial fib withWPW. I would just cardiovert electrically."
Smith: the rhythm is irregularly irregular without P-waves. There are delta waves and polymorphic QRS (but NOT polymorphic VT!). So this looks like WPW with Atrial fibrillation. What is unusual is that the rate is not REALLY fast, as you expect when there is atrial fib with an accessory pathway. The shortest R-R inteval that I see is between the 6th and 7th beat and is 280 ms, which is not dangerously short.
Nevertheless, you NEVER want to give an AV nodal blocker to Atrial fib with WPW:
1. The reason to avoid AV blockers in WPW is that, in addition to blocking AVN, they actually enhance conduction via AP by shortening refractory period, which can produce VF.
2. Adenosine is considered safe for termination of AVRT in WPW, but the pro-arrhythmic effects of adenosine can rarely cause AF, so do not give AVN blocker to WPW unless you have defib pads placed.
The essential features of A Fib WPW are:
1. Irregularly irregular
2. Polymorphic
3. Wide
4. Some very short R-R intervals
Never give an AV nodal blocker to Atrial Fibrillation with WPW; it can result in ventricular fibrillation. This means NO calcium channel blocker, beta blocker, adenosine, or digoxin.
Cardioversion can be done pharmacologically (usually procainamide), but why would you want to do that? Only if you are unable to perform procedural sedation or if the patient refuses.
So electrical cardioversion was done (using etomidate sedation. I prefer low dose propofol, just enough for amnesia, but not enough to result in serious hypotension).
Here is the post cardioversion ECG:
Electrophysiology note: "In the context of pre-excited atrial fibrillation, we would recommend proceeding with mapping and ablation of accessory pathway (particularly given high risk features including his shortest pre-excited R-R interval is < 250 ms). It does appear likely that his pathway may anteroseptal, which does increase risk of damage to AV node."
More explanation from electrophysiology:
"ECG only records 10-seconds worth of data, therefore long rhythm strip is essential to make sure ample data is available. Fortunately in the stabilization room, they had recorded a long rhythm strip (Smith: not seen by me and not shown) during atrial fibrillation and some R-R intervals were very short approaching 250 msec."
He was taken for immediate ablation that day in the EP lab, but (explanation from electrophysiology) this ECG was recorded:
Electrophysiolgy explains: "These accessory pathways can be very superficial fibers and during the first procedure, it got mechanically “bumped” before turning on ablation and therefore NO ABLATION WAS PERFORMED in absence of preexcitation, given high risk location. Despite of waiting for an hour pathway conduction did not come back (but they do invariably come back after such mechanical bump). Therefore repeat procedure was performed with Cryo-ablation after the accessory pathway conduction had returned."
The next morning, this ECG was recorded:
The delta waves are back. There is recurrent pre-excitation.
The Ablation was done.
He was taken for another ablation and this ECG was recorded:
MY Comment, by KEN GRAUER, MD (5/8/2024):
- For clarity in Figure-1 — I've labeled the first 2 tracings in today's case.
- As I illustrated in My Comment at the bottom of the page in the March 6, 2020 post of Dr. Smith's ECG Blog — while not infallible, the finding of a very short RP' interval suggests the mechanism of the reentry SVT rhythm is AVNRT, in which the impulse travels back to the atria over the "fast" AV nodal pathway. This is because when the reentry circuit is entirely contained within the AV node — it takes minimal time to return to the atria.
- In contrast — the finding of a moderately long RP' interval suggests that the mechanism of the reentry SVT rhythm is orthodromic AVRT, in which a "concealed" AP may be participating in the reentry pathway. Because the AP lies outside of the AV node — the time to circulate around the reentry pathway and conduct back to the atria (retrograde) is longer than when the entire reentry circuit is contained within the AV node.
- IF you look for retrograde P wave conduction during a regular SVT rhythm — You'll begin to find it much more often than you might have imagined! On occasion — recognizing retrograde conduction may provide a KEY clue to the mechanism of a tachycardia.
- To LOOK for retrograde P waves: — i) Look in the inferior leads for a small negative notch that occurs at the very end of the QRS, or fairly soon thereafter; or, ii) Look for a small positive notch in lead aVR and/or lead aVL and/or lead V1; and, iii) Confirm that the notching you identified during the regular SVT rhythm truly reflects retrograde atrial activity (rather than being a part of the QRS or the result of artifact) — by noting that this notching is no longer present after conversion to sinus rhythm. (My Figure-2 in the March 6, 2020 post illustrates this confirmation).
- As shown in Figure-1 — the rhythm in today's initial ECG is a regular SVT (ie, Narrow-complex tachycardia) at ~190/minute, without sinus P waves.
- I initially thought the small negative notch at the very end of the QRS in lead II — and the small positive notch at the very end of the QRS in lead V1 — both represented retrograde P waves with a very short RP' interval (within the RED circles in these leads). If so — this would strongly suggest AVNRT of the "slow-fast" type (which is by far the most common form of AVNRT) as the mechanism of today's initial rhythm.
- That said — I thought the more-pointed-than-expected negative deflections in leads III and aVF — and the pointed tip of the upright T wave in lead aVL — might represent retrograde P waves, in which case the RP' interval would instead be moderately long (within the BLUE circles in these leads).
- BOTTOM Line: Given conflicting findings regarding my search for potential retrograde atrial activity — I could not distinguish between AVNRT vs orthodromic AVRT on the basis of ECG #1 alone. Sometimes you can distinguish between AVNRT vs orthodromic AVRT — but not in today's initial tracing.
- WPW is recognized on ECG by the presence of 3 Findings: i) A short PR interval; ii) Delta waves in a number of leads; and, iii) QRS widening.
- It's important to appreciate that patients with an AP may not always manifest these 3 findings that are characteristic of complete or predominant preexcitation. Instead — Patients with an AP may at times manifest partial or even no preexcitation (with the relative percentage of impulses traveling over the AP vs the normal AV nodal pathway being highly variable). IF the relative amount of preexcitation at any given time is minimal — then delta waves, PR interval shortening, and QRS widening may be barely (if at all) detectable.
- APs may conduct forward (anterograde) and/or backward (retrograde). While APs are usually capable of conducting in both directions — forward or backward conduction may not be possible in some patients. This leads to the concept of a "concealed" AP — in which only retrograde conduction is possible over the AP.
- Up to 15% of patients with a regular reentry SVT rhythm who are referred for catheter ablation may have a "concealed" AP, in which delta waves are never seen because forward (anterograde) conduction over their AP is not possible (Pappone and Santinelli — ESC: July, 2018).
- KEY Point: Synthesizing the concepts in the above bullets means that a significant percentage of the time when treating a new patient with a regular reentry SVT rhythm, but without clear sign of atrial activity — that despite never seeing delta waves, the patient may have a concealed AP (ie, that rather than AVNRT — the regular SVT may be orthodromic AVRT).
- The "good" news — is that initial treatment of such patients with a regular reentry SVT rhythm is the same (ie, Adenosine, Verapamil/Diltiazem, ß-Blocker) — because AV nodal blocking agents will successfully interrupt the reentry circuit in both AVNRT and orthodromic AVRT.
- The "less good" news — is that in up to 1/3 of patients with orthodromic AVRT — spontaneous AFib may develop at some point — presumably predisposed by "triggering" of AFib by AP-mediated reciprocating tachycardia (Ma et al — Exp Clin Cardiol 9(3): 196, 2004 — and Silverman et al. in J Investig Med: Jan, 2018). And, as per Dr. Smith — use of AV nodal blocking agents (ie, Adenosine, Verapamil/Diltiazem, ß-Blocker) are contraindicated in patients with AFib and WPW — because blockade of the normal AV nodal pathway may result in further acceleration of anterograde conduction over the AP, which may result in deterioration of the rhythm to VFib.
- The other "less good" news — is at least the theoretical risk that using an AV nodal blocking agent to treat a regular SVT might precipitate AFib if the patient had a "concealed" AP (ie, if instead of AVNRT — the rhythm was orthodromic AVRT). Fortunately — precipitation of AFib by giving an AV nodal blocking agent to a reentry SVT that turns out to be orthodromic AVRT is rare (and consensus remains to treat reentry SVT rhythms with AV nodal blocking agents).
- As per Dr. Smith — the rhythm in ECG #2 is irregularly irregular without P waves. While I hesitate in diagnosing delta waves in the absence of sinus P waves (because LBBB conduction may sometimes manifest initial QRS slurring) — the additional features of changing QRS morphology — and the finding of some very short R-R intervals alternating with some unexpectedly longer R-R intervals (ie, between beats #5-6) in this younger adult — suggested WPW with AFib (although definitive diagnosis of WPW was not made until the 3rd ECG was obtained, which showed return of sinus rhythm with short PR, delta waves and a similar-looking wide QRS).
- PEARL #1: As we have highlighted in previous posts (See the March 11, 2020 post) — WPW can be immediately diagnosed when you see AFib with a wide QRS and an extremely rapid ventricular response (that at times attains a rate of between ~220-250/minute!).
- Unlike PMVT (PolyMorphic Ventricular Tachycardia) in which QRS morphology usually changes dramatically from one beat to the next — the changing QRS morphology typically seen in WPW with AFib tends to be more subtle (due to modest variation in the relative percentage of preexcitation).
- PEARL #2: Not all patients with WPW are at high risk of developing potentially life-threatening tachyarrhythmias. The risk of developing VFib during AFib in a patient with WPW is greatly increased when the SPERRI (Shortest Pre-Excited R-R Interval) measures below 220-250 msec. This corresponds to a shortest R-R interval that is barely more than one large box in duration. We do not see this in ECG #2 — as the shortest R-R interval is 7 little boxes in duration ( = 280 msec. — as I've labeled between beats #6-7).
- How fast the ventricular response will be in association with AFib in a patient with WPW will depend on anterograde conduction properties of the AP. The overall rate of AFib in ECG #2 is ~150/minute (ie, There are 25 beats in the 10 second long lead II rhythm strip ==> 25 X6 = 150/minute). Since the ventricular response in ECG #2 is comparable to the rate range for any patient who develops new-onset AFib — definitive diagnosis of WPW was not made in today's case until the 3rd ECG was obtained.
- Even though the SPERRI value during AFib in today's case was not below 250 msec. — catheter ablation was indicated because this younger man was very symptomatic with not just one, but two WPW-related tachyarrhythmias (orthodromic AVRT and AFib).
- It is possible to have more than a single AP! (Goyal et al — StatPearls: July, 2023). While multiple APs in a given patient is not common — I initially wondered if that might be a possibility in today's patient, given the need for repeat ablation the next day. That said — the fact that morphology of the wide QRS was virtually identical in sinus rhythm after each ablation suggested this patient did not have more than a single AP (and in Dr. Smith’s discussion, under Electrophysiology Explains — we learn the reason the EP cardiology repeated the procedure the next day).
- Finally — Did you notice the very tall T waves in multiple leads after each ablation? This finding is typical for a post-ablation memory T wave pattern — which is often considered evidence of a successful ablation (Silverman et al — J Investig Med: Jan, 2018).







-USE.png)













-USE%20copy.png)


-USE.png)