This case comes from Jon B. Cole, one of our EM faculty and unparalleled toxicologist, and director of the Minnesota Poison Control Center.
@jonbcole2 https://twitter.com/jonbcole2
Here is his incredible list of publications for early career, with h-index of 18 and i10 index of 33!
Case
A young man was brought to the ED by friends with a complaint of progressive weakness to the point of extremity paralysis on arrival. He spoke no English and spoke a language for which only a phone interpreter was available. He was awake, alert, and oriented, but had 1/5 strength in all 4 extremities, such that they needed to hold the phone to his ear for him. He was areflexic.
Ventilations were rapid and shallow, but adequate.
He denied head or neck trauma, or neck pain. He did say that something like this had happened before in his home country.
Dr. Cole suspected the diagnosis and rapidly obtained a 12-lead ECG before any other test could be obtained:
Large U-waves confirm the diagnosis of hypokalemic periodic paralysis (HPP). The K returned at 1.4 mEq/L and K was given po and IV. The patient was admitted to the ICU.
Mg was normal and phosphate was very low.
@jonbcole2 https://twitter.com/jonbcole2
Here is his incredible list of publications for early career, with h-index of 18 and i10 index of 33!
Case
A young man was brought to the ED by friends with a complaint of progressive weakness to the point of extremity paralysis on arrival. He spoke no English and spoke a language for which only a phone interpreter was available. He was awake, alert, and oriented, but had 1/5 strength in all 4 extremities, such that they needed to hold the phone to his ear for him. He was areflexic.
Ventilations were rapid and shallow, but adequate.
He denied head or neck trauma, or neck pain. He did say that something like this had happened before in his home country.
Dr. Cole suspected the diagnosis and rapidly obtained a 12-lead ECG before any other test could be obtained:
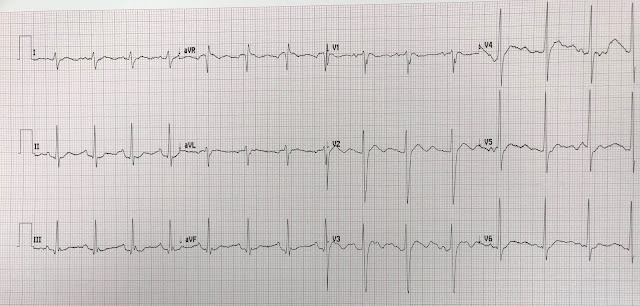 |
| And the diagnosis was made. What is it? |
Large U-waves confirm the diagnosis of hypokalemic periodic paralysis (HPP). The K returned at 1.4 mEq/L and K was given po and IV. The patient was admitted to the ICU.
Mg was normal and phosphate was very low.
The potassium was repleted in the ICU to a total of 170 mEq with resolution of symptoms (this could be hazardous!). He was monitored overnight observed for rebound hyperkalemia.
It is important to understand that with hypokalemic periodic paralysis, the total body K is not depleted. Instead, it has all gone into the cells. When it exits the cells for the extracellular space, then intravascular space, the K will rise, and sometimes dangerously if exogenous K has been given.
Potassium remained normal with 4.4 mEq/L on discharge without telemetry events. Nephrology consulted and and patient counseled about triggers for hypokalemic periodic paralysis in setting with normal thyroid studies. Counseled to avoid heavy carbohydrate diet and IV dextrose. Patient verbalized understanding and was discharged with potassium as needed.
It is important to understand that with hypokalemic periodic paralysis, the total body K is not depleted. Instead, it has all gone into the cells. When it exits the cells for the extracellular space, then intravascular space, the K will rise, and sometimes dangerously if exogenous K has been given.
Potassium remained normal with 4.4 mEq/L on discharge without telemetry events. Nephrology consulted and and patient counseled about triggers for hypokalemic periodic paralysis in setting with normal thyroid studies. Counseled to avoid heavy carbohydrate diet and IV dextrose. Patient verbalized understanding and was discharged with potassium as needed.

Was the qrs notching in lead v1 a result of this condition?
ReplyDeleteLiam — Please see my response to Anonymous just below — :)
DeleteAre the QRS notches in v1 a result of this acute issue?
ReplyDelete@ Liam & Anonymous — I do not believe that the notching in the QRS of lead V1 is related to the hypokalemia that was present in this case, or to the condition known as HPP. There is a “forme fruste” of IRBBB (incomplete RBBB) — in which the QRS is not wide — there are terminal S waves in lateral leads I and V6 — and instead of an rSr’ in lead V1, what you have is an rS-notch, as we do here. An rSr’ complex is common (and often NOT abnormal) in many young and healthy individuals, simply due to relative delay in depolarization of the RV outflow track with respect to depolarization of the LV. With a form “fruste” (ie, “frustrated”, or not quite complete IRBBB pattern) — there is a change in the depolarization vector, but not enough to establish an r’.
Delete